Nerve injury is common in multiple trauma, both of the spinal cord and other nerves. Cervical spine injury is common in patients with moderate to severe head injury.
The first priority is the Primary Survey:
- Airway and Cervical Spine
- Breathing
- Circulation
- Disability
- Exposure
Anatomy[edit | edit source]
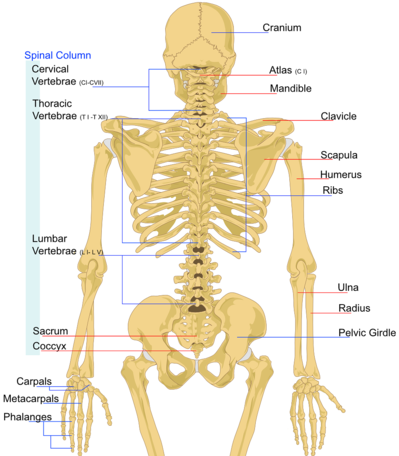
The Vertebral Column[2][edit | edit source]
Consists of 33 Vertebrae:[3]
- 24 Articulating
- Cervical = 7
- Thoracic = 12
- Lumbar = 5
- 9 Fused
- Sacral = 5
- Coccygeal = 4
Musculature of the Back[edit | edit source]
The Spinal Cord[7][edit | edit source]
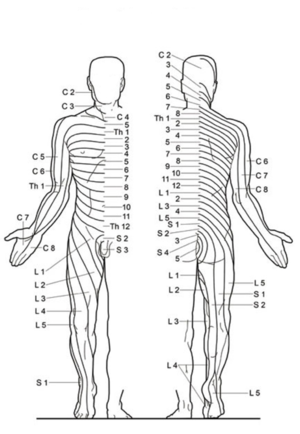
There are a Total of 31 Paired Spinal Nerves:[3]
- Cervical = 8
- Thoracic = 12
- Lumbar = 5
- Sacral = 5
- Coccygeal = 1
Spinal Cord Injury[8] (SCI)[edit | edit source]
Classification[edit | edit source]
Complete SCI[edit | edit source]
Consists of:
ABSOLUTE LOSS of Sensory AND Motor Function
BELOW the Level of Injury
Incomplete SCI[9][edit | edit source]
- Central Cord Syndrome[10]
- Anterior Cord Syndrome[11]
- Brown-Sequard Syndrome[12]
- Posterior Cord Syndrome[13]
- Cauda Equina Syndrome[14]
- Conus Medullaris Syndrome[15]
Assessment[edit | edit source]
Examination of spine-injured patients must be carried out with the patient in the neutral position (i.e. without flexion, extension or rotation) and without any movement of the spine.
The patient should be:
- Log-Rolled
- Appropriately Immobilised
- Manual In-Line Immobilisation
- OR
- Stiff Neck Cervical Collar, Sandbags and Tape
- Manual In-Line Immobilisation
With vertebral (bony) injury, which may be associated with spinal cord injury, look for:
- Local tenderness along the back
- Deformities and stepping
- Swelling and bruising
Clinical findings indicating injury of the cervical spine include:
- Difficulties in respiration (diaphragmatic breathing - check for paradoxical breathing)
- Floppy limbs and no reflexes
- Loose anal sphincter and loss of sensation in perineum
- Urinary and bowel incontinence or retention
- Neurogenic Shock: Hypotension with bradycardia (without hypovolaemia or blood loss)
Assessment of the Level of Spinal Injury[edit | edit source]
If the patient is conscious, ask the patient questions about sensation in the limbs and on the torso - note where the sensation changes
Ask the patient to do minor movements of the upper and lower limbs, starting with the fingers and toes - note where there is no movement and what movements the patient can do.
If Possible and Appropriate - Undertake Complete Neurological Examinations:
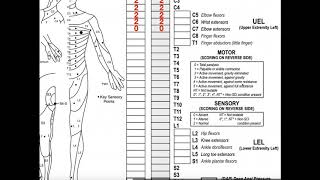
International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)[edit | edit source]
This tool represents the gold standard for assessment and documentation of spinal cord injury.[18] It is produced by the American Spinal Injury Association (ASIA), and the International Spinal Cord Society (ISCoS), the most recent version was produced in 2019.[18]
It serves as an extremely useful tool, to ensure that assessment and documentation of affected dermatomes and myotomes remains consistent.
For a downloadable PDF version of the 2019 ISNCSCI Worksheet,[19] please visit: https://asia-spinalinjury.org/
-
Page 1 of the ISNCSCI Worksheet: Indicates Dermatomes and Corresponding Assessment Locations, as well as Key Myotomes and Corresponding Assessment Movements.
-
Page 2 of the ISNCSCI Worksheet: Describes Muscle Function and Sensory Grading Scores, the ASIA Impairment Scale (AIS), and an Overview of the Steps of Classifying Spinal Cord Injuries.
X-Rays[21][edit | edit source]
All patients with a suspicion of cervical spine injury should have an AP and a lateral neck X-ray with a view of the atlantoaxial joint.
All seven cervical vertebrae and the junction with T1 must be seen on the AP and lateral views.
Management[edit | edit source]
Stepwise management of spinal injury:
- Stabilise the airway, breathing and circulation
- Immobilise the cervical spine with a hard collar, sand bags or whatever you have available
- Keep the patient lying flat on the back and in a neutral position
- Pain relief and anti-nausea medication if available
- Keep the temperature stable
- Insert a urinary catheter
- Transport the patient for surgical care in a neutral position; do not sit them up
Associated Conditions[edit | edit source]
Spinal Shock[edit | edit source]
Clinical Features[24][edit | edit source]
- Initial
- Areflexia
- Flaccidity
- Later
- Spasticity
Clinical Course[25][edit | edit source]
- Areflexia
- Initial Reflex Return
- Initial Hyperreflexia
- Spasticity
NOT a Form of Circulatory Collapse
Neurogenic Shock[26][edit | edit source]
Clinical Features[27][28][edit | edit source]
- Hypotension
- Refractory Despite Adequate Fluid Resuscitation
- Bradycardia
Pathophysiology[edit | edit source]
- Typical Level of Injury is T6 Vertebrae and Above[29]
- Autonomic Dysfunction → DISTRIBUTIVE Shock:[27]
- Parasympathetic Function = PRESERVED → Inappropriate Bradycardia
- Sympathetic Function = ABSENT→ Inappropriate Vasodilation → Loss of Preload → Hypotension
Management[29][edit | edit source]
- RULE OUT Another Cause of Shock
- ENSURE Adequate Resuscitation
- CONSIDER[30] - If Available:
- Vasopressors
- Inotropes
- Chronotropes
- ↑ https://www.youtube.com/watch?v=s8WfisaAY6Q&ab_channel=AnatomyZone
- ↑ https://teachmeanatomy.info/back/bones/vertebral-column/
- ↑ 3.0 3.1 https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Anatomy-of-the-Spine-and-Peripheral-Nervous-System#:~:text=There%20are%2031%20pairs%20of,other%20exits%20on%20the%20left.
- ↑ https://teachmeanatomy.info/back/muscles/superficial/
- ↑ https://teachmeanatomy.info/back/muscles/intermediate/
- ↑ https://teachmeanatomy.info/back/muscles/intrinsic/
- ↑ https://teachmeanatomy.info/back/nerves/spinal-cord/
- ↑ https://www.orthobullets.com/spine/2006/spinal-cord-injuries
- ↑ https://www.orthobullets.com/spine/2008/incomplete-spinal-cord-injuries?hideLeftMenu=true#popup/image/122920
- ↑ https://radiopaedia.org/articles/central-cord-syndrome?lang=gb
- ↑ https://radiopaedia.org/articles/ventral-cord-syndrome?lang=us
- ↑ https://radiopaedia.org/articles/brown-sequard-syndrome-1?lang=gb
- ↑ https://radiopaedia.org/articles/dorsal-cord-syndrome?lang=gb
- ↑ https://radiopaedia.org/articles/cauda-equina-syndrome?lang=gb
- ↑ https://radiopaedia.org/articles/conus-medullaris-syndrome?lang=gb
- ↑ https://www.youtube.com/watch?v=0hhcxaeOCYs&ab_channel=GeekyMedics
- ↑ https://www.youtube.com/watch?v=-7ERNH_o5Ss&ab_channel=GeekyMedics
- ↑ 18.0 18.1 ASIA and ISCoS International Standards Committee. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)—What’s new?. Spinal Cord 57, 815–817 (2019). https://doi.org/10.1038/s41393-019-0350-9
- ↑ https://asia-spinalinjury.org/wp-content/uploads/2019/10/ASIA-ISCOS-Worksheet_10.2019_PRINT-Page-1-2.pdf
- ↑ https://www.youtube.com/watch?v=LErgPVcgHW0&ab_channel=CatalystUniversity
- ↑ https://www.radiologymasterclass.co.uk/tutorials/musculoskeletal/x-ray_trauma_spinal/x-ray_c-spine_normal
- ↑ https://www.youtube.com/watch?v=XcU6g_ppWRI&t=1s&ab_channel=MedicalEducationLeeds
- ↑ https://www.youtube.com/watch?v=Stc5mzIFJBY&ab_channel=MedicalEducationLeeds
- ↑ Robert A. Boland and others, Adaptation of motor function after spinal cord injury: novel insights into spinal shock, Brain, Volume 134, Issue 2, February 2011, Pages 495–505, https://doi.org/10.1093/brain/awq289
- ↑ Ditunno, J.F., Little, J.W., Tessler, A., Burns, A.S. Spinal shock revisited: a four-phase model. Spinal Cord. 2004; 42: 383–395. https://doi.org/10.1038/sj.sc.3101603
- ↑ https://criticalcarenow.com/neurogenic-shock/
- ↑ 27.0 27.1 Stein, D.M., Knight, W.A. Emergency Neurological Life Support: Traumatic Spine Injury. Neurocrit Care 2017; 27 (Suppl 1): 170–180. https://doi.org/10.1007/s12028-017-0462-z
- ↑ Go, S. Spine Trauma. In: Tintinalli, J. E., Ma, O. J., Yealy, D. M., Meckler, G. D., Stapczynski, J. S., Cline, D. M., Thomas, S. H. (eds.) Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. New York: McGraw Hill Education, 2020. p.1696-1714.
- ↑ 29.0 29.1 Parra, M.W., Ordoñez, C.A., Mejia, D., Caicedo, Y., Lobato, J.M., Castro, O.J., Uribe, J.A., Velasquez, F. Damage control approach to refractory neurogenic shock: a new proposal to a well-established algorithm. Colombia Medica. 2021; 52(2): e4164800. https://doi.org/10.25100%2Fcm.v52i2.4800
- ↑ Kanter, J., DeBlieux, P. Pressors and Inotropes. Emergency Medicine Clinics of North America. 2014; 32(4): 823-834.
- ↑ https://www.youtube.com/watch?v=d2NCMoJZe-Q&ab_channel=ICUAdvantage