Limb trauma management is based on the PTC manual handbook, and the need to establish catastrophic haemorrhage[1] control as a principle tenant of the Primary Surveys[2] ABCDE strategy. Peripheral haemorrhage is a preventable cause of early mortality and early treatment of limb injuries reduces late morbidity.
Learning Agenda[edit | edit source]
- Understand the structured approach to the patient with limb injury
- Be able to treat limb injuries and prevent further injury
Anatomy[edit | edit source]
Please consider reviewing the relevant anatomy of the lower limb:
- Bones[3]
- Vasculature
- Nervous Supply[14]
“A fracture is a soft tissue injury that happens to have a broken bone beneath”
Principles[edit | edit source]
Management decisions are based on a complete history and assessment of injuries.
Assessment[edit | edit source]
ABC[edit | edit source]
Look[edit | edit source]
- Skin colour
- Grazes, wounds and bleeding sites
- Limb alignment, deformities and swelling
Feel[edit | edit source]
- Temperature
- Tenderness
- Pulse assessment[15] - Comparing:
- Proximal and distal to a fracture
- Contralateral pulses
- Crepitus (on joint movement)
Move[edit | edit source]
- Active and passive movements - appreciate associated levels of pain
Management involves[edit | edit source]
- ABC
- Haemorrhage control
- Basic Fracture management
- Pain Relief
Aim[edit | edit source]
- Maintain peripheral perfusion
- Prevent skin necrosis and infection (sterile wound dressings)
- Prevent damage to peripheral nerves
Special Issues Relating to Limb Trauma[edit | edit source]
Haemorrhage Control[edit | edit source]
Blood loss from musculoskeletal trauma may not be obviously apparent hence the need to appreciate the significance of long bone injuries, particularly in the context of major soft tissue damage or open trauma.
STOP[16] the bleeding[edit | edit source]
- Fracture reduction (restore normal alignment, angulation and rotation profile)
- Traction, Splint or immobilisation
- Direct pressure over bleeding site (gauze can be augmented with circumferential elastic bandage)
- Tourniquet (if all else fails) and release as soon as possible (Life over Limb but consider temporary release at 1hour if definitive surgical time is beyond this)
- Tranexamic acid
Replace the blood loss[edit | edit source]
- Large transfusion protocol
- Crystalloid or Colloid agents
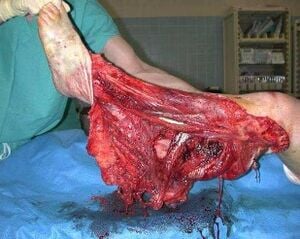
Open Fractures[17] and Joint Injuries[edit | edit source]
Any fracture or joint injury situated near a wound must be considered as “open”.
Principles of the treatment include:
- Prevent Infection with weight based Antibiotic dosing and Tetanus coverage as soon as possible
- Stop external bleeding, remove gross contaminants and cover with moist gauze
- Accurately describe the wound, noting any soft tissue and neuro-vascular involvement
- Reduce, Splint and Immobilise
- Relieve pain
- Early surgical consultation
Traumatic Amputation of Extremities[edit | edit source]
Management
- Wound/Stump
- Cover the wound with sterile gauze
- Amputated Limb
- Thoroughly wash amputated part with isotonic solution
- Wrap with moistened saline gauze
- Encase in moist saline towel
- Place into a sterile bag
Foreign Bodies[edit | edit source]
Deep penetrating foreign bodies should remain in situ until exploration in theatre.
Severe Complications[edit | edit source]
Compartment Syndrome[18][edit | edit source]
Definition[edit | edit source]
A destructive cascade characterised by local soft tissue trauma, subsequent oedema, bleeding and increased osseofascial compartment pressures. This decreases the perfusion gradient across tissue capillary beds, leading to cellular anoxia, neuro-muscle ischaemia, tissue necrosis and potentially death.
Assessment[edit | edit source]
Suspect it in patients that have pain out of proportion to the injury. It is frequently missed. The earliest and most important sign is increasing pain especially on passive stretching of the muscles. Loss of pulse or sensation are very late signs.
Management
Early detection and appropriate fasciotomy:
- Hand & Finger Compartments
- Forearm Compartments
- Upper Limb Compartments and Fasciotomy
- Proximal Lower Limb Fasciotomy[19]
- Distal Lower Limb 4-Compartment Fasciotomy[20]
- Foot Fasciotomy
Crush Syndrome[21][edit | edit source]
A severe, systemic, result of trauma and ischaemia, due to prolonged severe crushing of soft tissues. It principally affects skeletal muscle of the upper limbs, lower limbs and pelvis, with sensory and motor disturbances in the compressed limb.
- The limb may become tense, swollen and pulseless.
- Myoglobinuria and/or haemoglobinuria due to skeletal muscle destruction make the urine tea-coloured quite early on.
- Hypovolaemic shock,[22] acidosis and renal failure are present.
Management
The main goal of treatment is to prevent crush injury syndrome developing:
- Start IV fluids - Ideally before the limb is freed and decompressed
- Insert a urinary catheter
Scenarios[edit | edit source]
References[edit | edit source]
- ↑ https://litfl.com/major-haemorrhage-in-trauma/
- ↑ Primary Assessment
- ↑ https://teachmeanatomy.info/lower-limb/bones/
- ↑ https://teachmeanatomy.info/upper-limb/bones/humerus/
- ↑ https://teachmeanatomy.info/upper-limb/bones/radius/
- ↑ https://teachmeanatomy.info/upper-limb/bones/ulna/
- ↑ https://teachmeanatomy.info/upper-limb/bones/bones-of-the-hand-carpals-metacarpals-and-phalanges/
- ↑ https://teachmeanatomy.info/lower-limb/bones/femur/
- ↑ https://teachmeanatomy.info/lower-limb/bones/tibia/
- ↑ https://teachmeanatomy.info/lower-limb/bones/the-fibula/
- ↑ https://teachmeanatomy.info/lower-limb/bones/bones-of-the-foot-tarsals-metatarsals-and-phalanges/
- ↑ https://teachmeanatomy.info/lower-limb/vessels/arterial-supply/
- ↑ https://teachmeanatomy.info/lower-limb/vessels/venous-drainage/
- ↑ https://teachmeanatomy.info/lower-limb/nerves/
- ↑ https://www.youtube.com/watch?v=0qZ5-C13Ccs
- ↑ Hemorrhage Control
- ↑ https://teachmesurgery.com/orthopaedic/principles/open-fractures/
- ↑ https://litfl.com/compartment-syndrome/
- ↑ https://www.youtube.com/watch?v=2ml3uBXUOAg
- ↑ https://www.youtube.com/watch?v=yhIEXC3JrYs
- ↑ https://litfl.com/crush-syndrome/
- ↑ https://www.theresusroom.co.uk/shock-in-trauma/
- ↑ https://www.youtube.com/watch?v=XcU6g_ppWRI
- ↑ https://www.youtube.com/watch?v=Stc5mzIFJBY