This module allows surgical practitioners to become more confident and competent in Orthoplastic reconstruction by removing contaminated debris and all devitalized tissue, stabilizing the skeleton and covering the soft tissue defect. This should reduce the bacterial burden and available substrate for microbial colonization, resulting in fewer deep surgical site infections. This will lead to improved patient outcomes in Sub-Saharan Africa (SSA). The situation in Rwanda is of grave concern as only two trained plastic surgeons and three plastic surgeon residents treat 13.28 million people. Currently, Rwanda has a surgical workforce of fewer than 2 surgeons, anesthesiologists, and obstetricians (SAOs) per 100,000 population, and investing in the training and education of the surgical workforce is the best way to increase the number of surgical interventions in Rwanda.
From 1990-2018 the average number of amputations in Sub-Saharan Africa (SSA) is 625,000 per year. The leading causes of amputation in SSA are vascular disease 50.1%, trauma 48.1%, and cancer 1.5%. Orthoplastic reconstruction aims to reduce the need for amputation and provides a treatment plan that combines orthopedics and plastic surgery. This cross-discipline treatment approach is the perfect training and educational module for a country with 2 plastic surgeons for 13.28 million people. The orthoplastic approach to extremity reconstruction is a collaborative model of orthopedic and plastic surgeons working together to expedite and optimize the care of patients needing lower extremity reconstruction.
Educational Learning Theory:
Proposed Learning Theory is a blending of deliberate practice, adaptive flexibility, and Kolb’s Experimental Learning Theory (ELT). Ericsson, Krampe, and Tesch-Römer (1993) established the theoretical framework of deliberate practice. Specifically, the authors (1993) define expert performance as the result of an individuals’ prolonged efforts to improve performance while negotiating motivational and external constraints (p. 363). Moulaert, Verwijnen, Rikers, and Scherpbier, (2004), explain that two distinct motivations are prevalent to mastery skill obtainment motivation and external information. Simply, if a learner is motivated and provided time to utilize outside educational resources (journals, books, videos, etc.) they can achieve proficiency through deliberate practice with the appropriate training materials (2004). Moreover, Ericsson, Prietula, and Cokely, (2007) clearly state the historical evidence that experts are made, not born. Further, their conclusions are based on rigorous research that looked at exceptional performance using scientific methods that are verifiable and most of all reproducible (2007).
Learning Objectives[edit | edit source]
This training module combines virtual and physical simulation in order to impart knowledge and skills for clinical competency in Orthoplastic reconstruction.
Within the module, learners will direct themselves through a comprehensive curriculum covering the indications, design, complications, and surgical techniques relevant to performing Orthoplastic reconstruction. After successfully completing the module, learners will:
- Understand the function of and indications for Orthoplastic reconstruction
- Understand the principles of Orthoplastic reconstruction design
- Describe and implement the stepwise surgical technique for performing Orthoplastic reconstruction
- Understand the complications of Orthoplastic reconstruction and how to avert them.
Syllabus[edit | edit source]
- Plastic Approach
- Orthopedic Approach
- Virtual Simulator
- Orthoplastics Reconstruction Physical Simulator Guide
- Ex-Fix Simulation - Procedure Steps
- Fasciocutaneous Flap Simulation Steps
- AmoSmile Home
How to follow this Syllabus[edit | edit source]
The Orthoplastic reconstruction training module is contained within the free and easy-to-use Amosmile smartphone application. Begin using the AmoSmile app by creating your personal account. Next, select the Orthoplastic reconstruction module from the Module Menu.
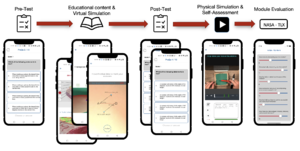
Within the Orthoplastic reconstruction module of the AmoSmile app, begin by completing a 20-question pre-module assessment to evaluate your baseline knowledge.
Review the carefully curated educational content contained within the Orthoplastic reconstruction module. This includes text, diagrams, and interactive graphics pertaining to the function, design, indications, complications, and surgical technique of Orthoplastic reconstruction.
After mastering the provided educational content, put your newly acquired knowledge to task using the virtual simulator. Here, you will be asked to perform a virtual Orthoplastic reconstruction within a simulated clinical scenario.
After completing the virtual simulation, complete an 80-question post-module assessment to evaluate your readiness to proceed in the course. A minimum passing score of 80% accuracy is required to qualify for continuation to the physical simulator.
Complete the video tutorial for constructing your physical simulator. You will then be guided through a simulated clinical scenario using your physical simulator. Stepwise self-assessment questions are integrated into the simulation to provide a performance feedback loop toward mastery learning. After completion, your score will be displayed alongside targeted guidance for additional review. Repeat the physical simulation until a perfect self-assessment score is achieved. You will then receive a Certificate of Completion, marking the conclusion of the module.
Along with the pre/post assessments, and virtual simulation self-assessments with directed learning feedback, learners must complete the SURG-TLX tool to aid in our continued development of this and other modules. Further, learners will complete the physical simulator with the OSATs and CCAT assessment tools and these tools will be used in conjunction with case reports for clinical validation.
The learning design of the application, partnered with a physical simulator, is a perfect conduit to evaluate a learner’s clinical competency. Our system divides learning into four hierarchical processes that mirror Miller's pyramid: knowledge, application of knowledge, clinical skills competency, and clinical performance. This instructional design methodology is echoed across all four modules and was chosen for its flexibility. Our theory utilizes a strong instructional design methodology, with adult learning theories that will yield a positive clinical competency output through ubiquitous learning. The creation of both virtual and physical simulators provides a lifelike example of a clinical encounter where a novice learner can make mistakes and learn from past experiences without endangering patients. Each module course begins with an MCQ section with a threshold of 80% for passing (knowledge), a virtual simulation (application of knowledge), post-evaluations with self-directed feedback (clinical skills), and the final physical simulator (clinical performance).