
Our Modules[edit | edit source]
- Z-Plasty
- V-Y Advancement Flap
- Orthoplastic reconstruction
- How to make the NEW tissue-realistic physical simulator
Our Team[edit | edit source]
Team AmoSmile is a collaboration created for the Global Surgery Training Challenge (GSTC) comprised of individuals from Operation Smile and AmoDisc. The team includes surgical and clinical experts from across the world with experience in delivering high-quality essential surgical care for burns, trauma, and cleft conditions. The team also includes medical educators and technology experts with experience in building simulation-based solutions for medical and surgical education.
Mission: The AmoSmile mission is to facilitate confidence and competence in performing local flaps for the treatment of burns, trauma, cancer, and congenital anomalies.
Vision: Our vision is to provide high-quality and freely accessible training modules to expand the reconstructive surgery workforce in resource-constrained settings
The Problem[edit | edit source]
Patients in low- and middle-income Countries (LMICs) suffer a disproportionate burden of conditions amenable to treatment by reconstructive surgical procedures, including burns, trauma, infection, cancer, and congenital anomalies. Each year, these conditions affect 122 million people worldwide and result in a cumulative loss of 95 million disability-free life years - more than threefold the burden of the top five non-reconstructive surgical conditions combined. This is further compounded by the economic destitution that too often mars the lives of those living with untreated reconstructive conditions. Chronic pain and disability related to reconstructive conditions preclude the attainment of meaningful employment, nearly 70% of which requires manual labor. Reconstructive conditions resulting in disfigurement result in even further compromises to quality of life, due to social isolation and mental health disorders.
The situation in Rwanda is of grave concern as only two trained plastic surgeons and three plastic surgeon residents treat 13.28 million people. Currently, Rwanda has a surgical workforce of fewer than 2 surgeons, anesthesiologists, and obstetricians (SAOs) per 100,000 population, and investing in the training and education of the surgical workforce is the best way to increase the number of surgical interventions in Rwanda. One of the plastic surgeons, Dr. Furaha, states, “We do not have the accurate number of patients who need plastic surgery, but from some registry of the Ministry of Health, between 100 and 150 children are born with defects, and of course, they will have to be put on the waiting list which sometimes leads to death of some patients or others are crippled because their conditions were not treated early," Further, Professor Bekele states "We have seen that most training hospitals are based in big cities, and the rural communities are left out, we seek to increase these training into district hospitals which will make trainees reach more patients and also try to reduce this gap." In 2015, the Lancet Commission on Global Surgery (LCoGS) determined that more than five billion people worldwide lack access to safe, affordable, timely surgical, obstetric, and anesthesia (SOA) care.1 According to the LCoGS key messages, low- and middle-income countries (LMICs) are disproportionately affected by this deficit, with more than 95% of individuals living in LMICs lacking access to life-saving surgical care that results in nearly 17 million deaths from untreated surgical conditions. Although LMICs account for 84% of the global population, only 6.3% of all worldwide procedures are performed within these countries. Therefore, it is imperative to increase access to quality surgical care in LMICs through evidence-based approaches and community-driven solutions that address the significant burden of unmet surgical needs – a global initiative championed by the World Health Organization as part of their Sustainable Development Goals 2030 agenda. When we analyze the data organized by the Sociodemographic Index (SDI) and the Global Burden of Disease 2019 (GBD 2019), Rwanda is categorized as having a low SDI rank with n=328. Over the 29 years of data collected by GBD2019, an estimated 251,871,087 burns occurred, with 3,605,749 deaths and 248,934,130 DALYs. As of 2019, 78% of the burns, 89% of deaths, and 89% of all global DALYs occurred in Low to Middle SDI countries. [1]
Our Solution[edit | edit source]
A broad armamentarium of procedures exists for reconstructing defects arising from burns, trauma, infections, and cancer. These reconstructive procedures are largely derived from local flaps. The foundation of reconstructive surgery, local flaps involve the elevation and transfer of tissue to reconstitute an adjacent defect. Chief among their many benefits is their readiness to adaptation. Local flaps can be specifically tailored to meet the aesthetic and functional requirements of a seemingly infinite range of tissue defects, spanning all surgical subspecialties. Furthermore, they require only basic surgical instruments and modest operative time.
Task sharing is a powerful strategy by which to scale the surgical workforce and address the global burden of reconstructive conditions. In that spirit, we hope to utilize mixed-methods simulation as a means to extend the reach and impact of basic reconstructive techniques to non-reconstructive surgeons.
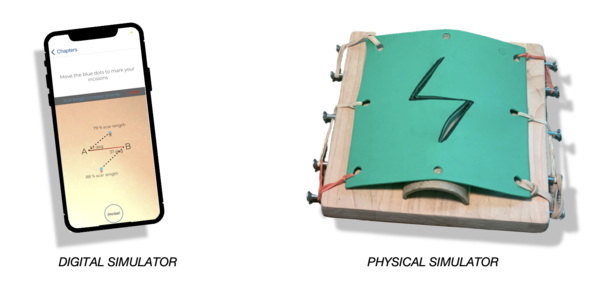
- The virtual component of our approach utilizes a mobile app that guides learners through a comprehensive surgical curriculum, including step-by-step simulations with dynamic competency tracking. This app is compatible with Apple and Android smartphones as well as all web browsers, which ensures uninhibited access irrespective of how users connect to the virtual platform. Furthermore, the app utilizes AWS app sync datastore technology, allowing data to stream to and from users' internal smartphone storage and our cloud-based servers regardless of internet connectivity.
- The physical component of our approach shifts the focus of learning from knowledge building to psychomotor skills acquisition. Our physical simulator is easily assembled from low-cost and locally-sourced materials to replicate the anatomy relevant to local flap techniques.
Taken together, our mixed-methods curriculum allows for any surgical practitioner – regardless of specialty – to master reconstructive techniques in an accessible, self-directed, and clinically-translatable manner.
The AmoSmile Smartphone App[edit | edit source]
AmoSmile training modules are all contained within a free and easy-to-use smartphone application. The AmoSmile app can be downloaded from both the Apple App Store and Google Play. Once downloaded, create your personal account to access the carefully curated curriculum within each module, including educational content, virtual and physical simulations, knowledge tests, and skills self-assessments.
Target User
This training platform is designed for any formally recognized surgical practitioner whose scope of practice includes the surgical treatment of wounds or defects that arise from burns, trauma, cancer, and/or infections. Users may be surgeons, obstetricians, clinical officers, or other healthcare practitioners who possess the accreditation to perform surgical procedures for reconstructive conditions like those mentioned above.
User Evaluation
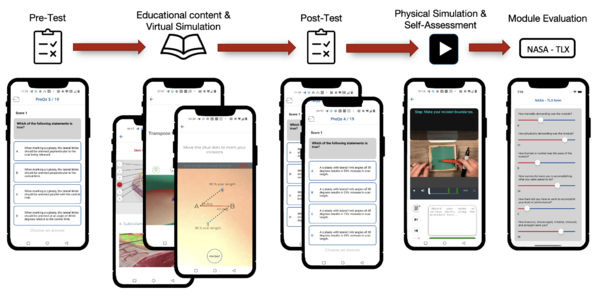
The learning design of the application, partnered with a physical simulator, is a perfect conduit to evaluate a learner’s clinical competency. Our system divides learning into four hierarchical processes that mirror Miller's pyramid: knowledge, application of knowledge, clinical skills competency, and clinical performance. This instructional design methodology is echoed across all four modules and was chosen for its flexibility. Our theory utilizes a strong instructional design methodology, with adult learning theories that will yield a positive clinical competency output through ubiquitous learning. The creation of both virtual and physical simulators provides a lifelike example of a clinical encounter where a novice learner can make mistakes and learn from past experiences without endangering patients. Each module course begins with an MCQ section with a threshold of 80% for passing (knowledge), a virtual simulation (application of knowledge), post-evaluations with self-directed feedback (clinical skills), and the final physical simulator (clinical performance).
The AmoSmile training platform prioritizes a multi-modal approach to user evaluation. Both our virtual and physical simulators provide guided feedback with quantitative data for productive practice and valuable reflective observation, as follows:
- Pre- and post-module assessments: Before beginning a module, users complete a pre-assessment to establish their baseline knowledge of the procedure at hand. After completing the virtual simulation, users then complete a post-test assessment to identify their mastery of the preceding content. Based on the delta in their scores, trainees are directed to review specific areas of the educational content in order to proceed to physical simulation.
- Physical simulator self-assessment: Within the physical simulator, users are prompted to perform a step-wise assessment of each preceding task. These integrated self-assessment questions ascertain competency in both foundational knowledge and psychomotor skills. Users must repeat the physical simulation until a perfect score on the integrated self-assessment is achieved.
- SURG Task Load Index: Users complete the SURG-TLX following the completion of the physical simulation. SURG-TLX allows users to provide self-reflective scores related to the physical and mental workload of performing the simulated procedure. The scale has been well-validated for over 40 years as a reproducible method for assessing skill acquisition in astronauts, surgeons, and other high-demand, high-skill professions. In addition to allowing for longitudinal tracking of users progress towards clinical readiness, SURG-TLX also provides useful design feedback for the continued improvement of AmoSmile content.
- For the clinical evaluation, we provide the Clinical Confidence Assessment Tool (CCAT) and the Objective structured assessment of technical skills (OSATS).
