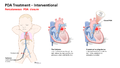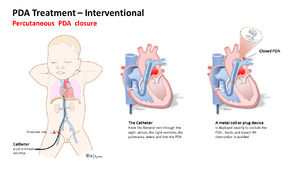
Patent ductus arteriosus (PDA) can be treated either interventionally in a cardiac catheterization lab, or surgically via ligation. This training is focused on the surgical approach to treatment, but trainees should also have basic familiarity with how a PDA is closed percutaneously.
Interventional Treatment[edit | edit source]
Surgical Closure[edit | edit source]
Preparation of skin: An antimicrobial scrub is preformed on thorax, spine, sternum and axilla from cervical spine to iliac crest. Chlorohexadine is not recommended for neonates under 1 months of age or premature infants.
Draping: Towels are placed at the vertebral column posteriorly, the sternum anteriorly, iliac crest to umbilicus inferiorly and suprasternal notch to axilla superiorly.
Incision: 4th intercostal space on left side.
Thermal Regulation: Room is warmed and patient is placed on a heater/cool mattress or Bair hugger.
Anatomical landmarks: 4th intercostal space, dividing the latissimus dorsi muscle but sparing the serratus anterior by retracting it anteriorly, a limited muscle sparing incision.
Structures requiring special attention to preserve and protect: The recurrent laryngeal nerve and the vagus nerve both lie in that area of the surrounding the aorta. The thoracic duct is the largest in the body and passes through the thoracic cavity from the abdomen and ascends through the chest aortic hiatus in the diaphragm. It ascends in the posterior mediastinum along the thoracic aorta (on the left), along the azygous vein (on its right) and put on the anterior esophagus.
Surgical Technique and Sequence of Procedure[edit | edit source]
- Using a 15 blade, a skin incision is made at the 4th intercostal space (left posterior lateral)
- Dividing the latissimus dorsi muscle and sparing the serrtas anterior muscle retracting it anterioirly with a army navy retractor.
- The lung is then retracted anteriorly.
- Providing exposure, a army navy retractor is used on muscle tissue, malleable retractors for lung tissue and fine debakeys used for cardiac tissue.
- The lymphatic channels are either preserved or ligated (depending on location and surgeon preference).
- The recurrent laryngeal and and vagus nerve are carefully preserved, by retracting and dissecting these structures with the mediastinal pleura anteriorly.
- The descending aorta, left subclavian artery, isthmus of the aorta and ductus arteriosus and transverse arch distal to the carotid artery are mobilized.
- Limited dissection is done; mainly to identify correctly all surround vessels.
- Occasionally vessel loops are used to retract the aorta, PDA or other vessels.
- Clip ligation: choose appropriate sized clips and fully occlude PDA towards pulmonary artery side of defect x 2 (clips not included in tool box).
- Ligation: using a right angle pass 2-0 silk x 2 around PDA tie towards pulmonary artery side of defect, be very gentle as tissue is fragile.
- Ligation and division: choose appropriate sized straight or angled vascular clamps place on the aortic and pulmonary artery side of vessels. Cut between leaving appropriate amount of tissue bilaterally to sew with 5-0 prolene to occlude vessels (vascular clamps not included in tool box). SPECIAL NOTE on Tissue Handling: PDA tissue is very fragile in nature, special attention needs to be made so no no tissue is torn or damaged (i.e., bleeding)
- Intraoperative monitoring: a increase in diastolic BP should be noted after ligation of the PDA.
- Pleura is closed
- A single chest tube is placed & attached to atrium.
- Muscle layers and skin are closed.
- Dressing placed