This page is intended as a supplementary resource to the didactic knowledge found in a paramedic program. It will cover all of the basic heart rhythms as well as potential causes and treatments but will not go into any significant depth behind the pathophysiology of each rhythm. If you are new to EKG rhythms, electrophysiology of the heart, or the electro-mechanics of ECG waveform propagation, it may be helpful to review the EKG section in the EMT Setup for ALS page or the Physiology of the Heart knowledge page prior to continuing on this page. This page will not cover advanced topics such as fusion beats, U-waves, or Osborne waves (J-waves).
A paramedic should have enough knowledge to identify each of these rhythms and treat them if necessary. The majority of the "treatment" knowledge will be covered in the didactic portion of a paramedic program. This page will assume that all rhythms are pulsing unless specifically stated. PEA (pulseless electrical activity) may be identified in the field by a ECG tracing of a rhythm normally associated with pulses but a pulseless patient. Any causes listed for a given rhythm are not the only causes, they have been presented as examples.
General EKG[edit | edit source]
Rate[edit | edit source]
A normal heartrate is between 60 and 100 beats per minute for a healthy adult. These numbers may vary due to cardiovascular exercise and effects of prescribed medications. If there is a question about the patient's rate and the patient is not in critical condition requiring immediate intervention, ask the patient what their normal heart rate is before assuming adverse pathology. All rates estimates on this page will be based upon adult physiology. Methods for determination of rate will be discussed in the 12 Lead EKG Interpretation page of this course.
Waveform Analysis[edit | edit source]
P-waves[edit | edit source]
P-waves indicate atrial depolarization and are normally found to be upright in the lead II analysis. Abnormalities include biphasic, inverted, or absent p-waves which may indicate atrial enlargement, junctional beats, or impaired conduction.
Q-waves̥̩[edit | edit source]
Q-waves are the first negative deflection of the QRS complex which indicates ventricular depolarization (assuming there is a subsequent positive deflection). In lead II, q-waves may be pathological (greater than 1 mm volume or 25̤ percent the height of the following R wave) which can indicate previous infarct. This is only useful when evaluating a 12 lead, as the pathological q-waves must be in contiguous or related leads.
R-waves[edit | edit source]
R-waves are the first positive deflection of the QRS complex which indicates ventricular depolarization. R-wave abnormalities such as a "rabbit ear" (RSR' complex) do not contribute to rhythm interpretation and are only useful when evaluating a 12 lead.
S-waves[edit | edit source]
S-waves are the negative deflection found following an r-wave. S-wave abnormalities such as slurring do not contribute to rhythm interpretation and are only useful when evaluating a 12 lead.
T-waves[edit | edit source]
T-waves indicate ventricular repolarization and are normally found to be upright in lead II analysis. T-wave inversion may be indicative of ischemia and a 12 lead should be performed for further analysis.
Interval Analysis[edit | edit source]
This section gives basic information on the intervals found in a normal rhythm tracing and will not cover the ST segment.
PR Interval[edit | edit source]
The PR interval is the time between the start of the p-wave and the start of the QRS complex. This interval is normally 0.12-0.20 seconds (120-200 milliseconds).
QRS Complex Duration[edit | edit source]
The duration of the QRS is normally less than 0.10 seconds (100 milliseconds) but a complex is only considered "wide" if the duration of the QRS complex is greater than 0.12 seconds (120 milliseconds). The QRS duration may be extended if there is a bundle branch block present for all following rhythms.
QT Interval[edit | edit source]
The QT interval is normally between 0.36 and 0.44 seconds (360-440 milliseconds) for a rhythm between 60-100 beats per minute. The QT interval will increase with bradycardia and decrease with tachycardia. A general rule is that if the QT interval is over half of the RR interval, it is prolonged.
RR Interval[edit | edit source]
The RR interval has no discreet values but is measured as the distance from one r-wave to another and should remain constant for a regular rhythm. Differing RR intervals indicates an irregular rhythm. The RR interval is not part of the "Intervals" section of the following rhythms as there is no concrete "normal" RR interval.
Rhythm Interpretation[edit | edit source]
Rhythm interpretation is covered in the didactic phase of paramedic programs and combines all of the above information and more to produce a method of identifying heart rhythms through specific characteristics. The minutiae of rhythm interpretation will not be covered on this page, instead, the following graphics serve to illustrate examples of common heart rhythms.
Sinus and Atrial Rhythms[edit | edit source]
Sinus and atrial rhythms are characterized as such because the impulse generation happens in the sinus node or the atria. This class of rhythms is the most commonly found within the normal human population and generally indicates a fairly healthy conduction system when compared to junctional or ventricular rates. With the exception of a 3rd degree heart block, any rhythm with p-waves of normal morphology and location may be considered a sinus rhythm.
"Normal" Sinus Rhythm[edit | edit source]
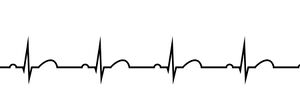
Overviewː A heart rhythm that follows normal conduction pathways. "Normal" is in quotes because a patient may be in a sinus rhythm with massive ST elevation, which is likely abnormal. The rhythm is a sinus rhythm but the patient is having a heart attack.
Rateː 60-100 bpm.
Intervalsː All within normal limits.
Causesː Normal physiological condition.
Treatmentsː None specific to the rhythm.
Sinus Bradycardia[edit | edit source]

Overviewː A heart rhythm that follows normal conduction pathways but with a slow rate.
Rateː Less than 60 bpm.
Intervalsː All within normal limits.
Causesː May be normal due to cardiovascular exercise. Myocardial infarction. Beta or Calcium channel blockers. Vagal stimulation.
Treatmentsː Occasionally fluid administration. Vasopressors/Chronotropes. Atropine. Transcutaneous/transvenous pacing.
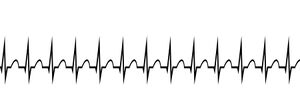
Sinus Tachycardia[edit | edit source]

Overviewː A heart rhythm that follows normal conduction pathways but with an increased rate.
Rateː Greater than 100 bpm.
Intervalsː All within normal limits.
Causesː Exercise. Sympathetic stimulation. Sympathomimetic drug use (cocaine, methamphetamine, albuterol, epinephrine). Compensated shock. Anxiety.
Treatmentsː Fluid administration. Beta or calcium channel blockers. Coaching/relaxation.
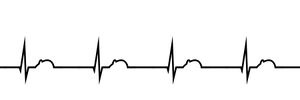
Sinus Arrhythmia[edit | edit source]

Overviewː A heart rhythm that follows normal conduction pathways but with an irregular rate due to changes in vagal simulation during respiration. Often confused with atrial fibrillation.
Rateː Irregular rate with RR interval difference greater than 0.12 seconds. May be fast or slow.
Intervalsː All within normal limits.
Causesː Respiration in some patients (may be normal).
Treatmentsː No specific treatment in the emergency setting. Treat bradycardias and tachycardias appropriately.
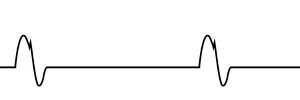
Sinus Arrest/Pause vs. Sinus Exit Block[edit | edit source]

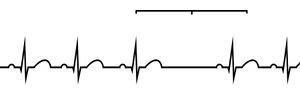
Overviewː Sinus arrest/pause and sinus exit block are two similar appearing ECG rhythms in which one or more full beats are dropped, including the p-wave (distinguishing these rhythms from a second degree type II AV block). A sinus exit block occurs when an impulse is not transmitted, but the next impulse is a multiple of the RR interval (i.e. the dropped impulse was "blocked"). In sinus pause or arrest, an impulse is dropped but the next impulse is not a multiple of the RR interval away from the first (i.e. the whole sinus note "paused" or "stopped").
Rateː Irregular rate with one or more dropped beats. May be fast or slow.
Intervalsː All within normal limits.
Causesː High vagal tone. Hypoxia. Hyperkalemia. Myocardial infarction. Side effects of drugs like digoxin. Sinus exit block may occasionally be found in well trained athletes as a normal physiological finding.
Treatmentsː No specific treatment in the emergency setting. Treat bradycardias and tachycardias appropriately.
Wandering Atrial Pacemaker[edit | edit source]

Overviewː A heart rhythm where there are 3 or more discrete atrial pacemaker locations. Distinguished by 3 or more p-wave morphologies found in a rhythm.
Rateː May be relatively regular, but is generally somewhat irregular due to shorter conduction distances/refractory phases of other pacemakers.
Intervalsː PR interval may be shortened if pacemaker is close to AV node.
Causesː Unclear, increased vagal tone or sinus node dysfunction may play a part.
Treatmentsː No specific treatment in the emergency setting. Treat bradycardias and tachycardias appropriately.
Multifocal Atrial Tachycardia[edit | edit source]

Overviewː A heart rhythm that is simply a wandering atrial pacemaker whose rate is above 100 bpm.
Rateː Greater than 100 bpm.
Intervalsː All within normal limits.
Causesː Decompensated chronic lung disease. CAD. Heart failure. Diabetes mellitus. Hypokalemia. Sepsis. Pneumonia.
Treatmentsː Treat cause of MAT.
Atrial Flutter[edit | edit source]

Overviewː A heart rhythm characterized by a 2ː1, 3ː1, or 4ː1 conduction resulting from a "trapped" electrical current. Note that while these are the most commonly found conduction ratios others do exist. Atrial flutter is a regular rhythm that can be easily identified by the obvious "sawtooth" or flutter waves produced.
Rateː Often times a whole number divided from 300. 75 (4ː1), 100 (3ː1), 150 (2ː1).
Intervalsː All technically within normal limits (flutter waves are technically p-waves).
Causesː "Trapped" electrical circuit causes atrial rate at around 300 bpm.
Treatmentsː No specific treatment in the emergency setting. Call online medical control if treatment questions exist.
Atrial Fibrillation[edit | edit source]

Overviewː A heart rhythm characterized by completely disorganized atrial electrical activity. Atrial fibrillation reduces cardiac output through loss of the "atrial kick" and can increase risk for clot formation and stroke. Atrial fibrillation is caused by many pacemakers within the atria simultaneously attempting to create a QRS complex. Due to the natural refractory period of the conduction system, these impulses will randomly create QRS complexes, creating an irregularly irregular rhythm.
Rateː Irregularly irregular. Rates may span large ranges and may be bradycardic (atrial fibrillation with slow ventricular response) or tachycardic (atrial fibrillation with rapid ventricular response). Manual measurement of pulse is the most effective for true determination of heart rate.
Intervalsː There are no p-waves and therefore no p-interval. R-R intervals are irregular. Other intervals remain unchanged.
Causesː May be normal for the patient as they age, previous damage to the heart, etc.
Treatmentsː Atrial fibrillation is often treated with blood thinners to reduce risk of stroke and may be treated with medications such as beta blockers to reduce rapid response. In the prehospital environment, atrial fibrillation has many possible treatments ranging from fluid administration, electrical cardioversion, and rate-control medications.
Supraventricular Tachycardia[edit | edit source]
A supraventricular tachycardia by name is a tachycardia in which the originating impulse starts above the ventricles. Since this could start in the atria, SVT is placed here. It will be discussed with the junctional rhythms.
Junctional Rhythms[edit | edit source]

Junctional rhythms are produced from the AV junction, as the name implies. A junctional rhythm will often arise due to an insufficiency of the SA node or proximal conduction system resulting in a loss of driving rate. This loss of atrial control of rate leads to the defining characteristics of junctional heart rhythmsː narrow complexes with abnormal or missing p-waves.
Missing p-wavesː As the p-wave is produced by atrial electrical activity, if the SA node and internodal pathways have been damaged by structural heart disease, a myocardial infarction, or other means, the p-wave may not be produced.
Flipped p-wavesː If the SA node is not producing an impulse but the internodal pathways are still patent, an impulse originating from the AV junction may sometimes travels in reverse, back up the internodal pathways towards the SA node. This retrograde conduction will produce a p-wave that is inverted and may be found before, during, or after the QRS complex depending on the origin of the pacemaker impulse.
Late p-wavesː Late p-waves may be found buried in the t-wave and may be upright (normal atrial conduction) or flipped (retrograde atrial conduction). Late p-waves that are upright may indicate a diseased SA node that still fires as it should but is late (this is incredibly rare, upright p-waves nestled in the t-wave are more commonly signs of a 3rd degree AV block). Late p-waves that are inverted are produced by the junctional pacemaker and are transmitted in the opposite direction as normal electrical movement.
Junctional Rhythm[edit | edit source]
Overviewː The stereotypical junctional rhythm may also be known as the junctional escape rhythm as it is causing the patient to "escape" death by utilizing the first of two backup pathways to keep the heart beating.
Rateː 40-60 bpm.
Intervalsː P-R intervals may not exist depending on presentation. All other intervals normal.
Causesː Heart disease, myocardial damage from MI or other causes.
Treatmentsː Treat symptomatic junctional rhythms via ACLS protocols if the underlying cause allows. Atropine, vasopressors, and pacing are all viable based on patient presentation.
Accelerated Junctional[edit | edit source]

Overviewː An accelerated junctional rhythm is the same as a junctional rhythm, just faster as the name suggests.
Rateː 60-100 bpm.
Intervalsː Same as junctional.
Causesː Same as junctional, with addition of possible shock states or medications.
Treatmentsː This patient's heart rate falls within the normal human physiological range. Treat the underlying cause, not the rhythm.
Junctional Tachycardia[edit | edit source]

Overviewː A junctional tachycardia is an accelerated junctional rhythm that is above the threshold for tachycardia.
Rateː Above 100 bpm.
Intervalsː Same as junctional. Some intervals may be normally shortened due to rate.
Causesː Same as junctional, with addition of possible shock states or medications.
Treatmentsː Do not attempt cardioversion, it is likely to be unsuccessful. Rate control as needed, but treat underlying cause before treating the rhythm.
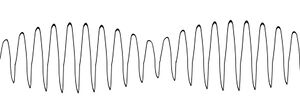
Supraventricular Tachycardia[edit | edit source]
Overviewː Supraventricular tachycardia, or SVT for short, is a junctional rhythm characterized by a rate of greater than 150 bpm. There are several possible etiologies for SVT, but some of the more common include a nodal re-entry loop where electricity circles around within the AV node and accessory pathway usage where a second conduction pathway allows for circular conduction (WPW or LGL, for example). SVT differs from VT because it is found with a narrow QRS complex, although SVT with aberrancy does exist.
Rateː Greater than 150 bpm.
Intervalsː The PR interval does not exist. All other intervals normal with respect to rate.
Causesː Congenital heart issues, idiopathic, excessive stimulant intake.
Treatmentsː Fluid administration and adenosine for stable SVT, electrical cardioversion for unstable SVT.
Ventricular Rhythms[edit | edit source]
Ventricular rhythms are characterized by large, abnormal QRS complexes caused by slow cell-to-cell depolarization in through the ventricular parenchyma. Ventricular rhythms are commonly found without p-waves and can be differentiated from junctional rhythms by their wide complexes.
Idioventricular[edit | edit source]
Overviewː An idioventricular rhythm is one where the SA and AV nodes are not transmitting due to disease or damage. In this scenario, the Purkinje fibers take up the slack and generate a beat.
Rateː 20-40 bpm.
Intervalsː No PR interval, prolonged QRS complex greater than 0.12 sec, other intervals generally normal for rate.
Causesː Myocardial damage.
Treatmentsː Atropine may be effective and may be attempted, but also may not work if the proximal conduction system is truly non-conducting. Therefore, pacing will likely be necessary for most truly symptomatic patients. Vasopressors may be effective if not contraindicated.
Accelerated Idioventricular[edit | edit source]
Overviewː An accelerated idioventricular rhythm is an idioventricular rhythm that is faster than 40 bpm but slower than 100 bpm.
Rateː 40-100 bpm.
Intervalsː No PR interval, prolonged QRS complex greater than 0.12 sec, other intervals generally normal for rate.
Causesː Same as idioventricular, with addition of possible shock states or medications.
Treatmentsː Same as idioventricular, but be wary of underlying causes that may be treatable in addition to the rhythm itself.
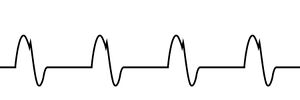
Ventricular Tachycardia (Pulsing and pulseless)[edit | edit source]
Overviewː Ventricular tachycardia (VT) is a potentially deadly pulsing rhythm and one of the shockable pulseless rhythms. Ventricular tachycardia comes in two forms, monomorphic (shown here) and polymorphic (an example of which is Torsades de Pointes shown below).
Rateː Greater than 100 bpm.
Intervalsː Often unable to calculate proper intervals due to increased QRS duration and speed of rhythm. Will generally be regular.
Causesː Cardiac arrest, hypoxemia, toxin ingestion, stimulant overdose, chronic heart disease, electrocution.
Treatmentsː For stable, pulsing VT amiodarone/lidocaine may be mixed and hung. For unstable, pulsing VT electrical cardioversion is indicated. For pulseless VT, defibrillation, epinephrine, and amiodarone/lidocaine are indicated with CPR.
Torsades de Pointes (Pulsing and pulseless)[edit | edit source]
Overviewː Torsades de Pointes (TDP) is a polymorphic VT that has a predictable pattern where the amplitude of the waveforms increases and decreases rhythmically while the direction of the waveform may switch. Similarly to monomorphic VT, TDP may be pulsing or pulseless.
Rateː Greater than 100 bpm.
Intervalsː Unable to be measured.
Causesː Hypo-calcemia/kalemia/magnesemia, Hyperkalemia, Long QT intervals, Congenital heart issues.
Treatmentsː Pulsing TDP may have magnesium sulfate or amiodarone/lidocaine hung based upon availability and local protocol if stable and unsynchronized electrical cardioversion if unstable. If pulseless, follow the same algorithm of CPR, defibrillation, and epinephrine as pulseless VT but substitute magnesium sulfate for amiodarone/lidocaine if available.
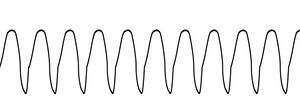
Ventricular Fibrillation[edit | edit source]
Overviewː Ventricular fibrillation is always pulseless and is characterized by a wavy ECG with no organized activity. There are two types of v-fib, coarse (larger waves) and fine (smaller complexes).
Rateː Unable to be determined. No pulse.
Intervalsː Unable to measure.
Causesː Electrolyte imbalance, R on T phenomenon, hypoxemia, hypothermia, trauma.
Treatmentsː CPR, epinephrine, defibrillation, repeat. Treat reversible causes as you find them.
Atrioventricular Blocks[edit | edit source]
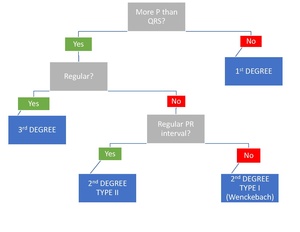
Atrioventricular blocks are caused by disease or damage to the AV node which may impinge or completely block transmission of impulses from the atria to the ventricles. Remember that with the exception of accessory pathways like those found in WPW or LGL there is electrical insulation between the atria and ventricles with the only point of crossing being the AV node. There are 3 degrees of AV blocks which can be easily differentiated by several characteristics, shown in Table 1. AV blocks have been the bane of many a student, so this flowchart will hopefully help with identification. The flowchart asks 3 questions that will always lead to the correct AV block if no other ectopy or underlying issues exist. These questions are as followsː
1. Are there more P waves than QRS complexes?
Of the 3 degrees of AV block, only one has a 1:1 ratio of P waves to QRS complexes, and that is the 1st degree heart block.
2. Is the rhythm regular?
Both 1st and 3rd degree heart blocks are regular, but 1st degree blocks were already ruled out. If a rhythm has more P waves than QRS complexes AND is regular, it is a 3rd degree heart block.
3. Is the PR interval constant?
A 2nd degree Type I heart block has a longer and longer PR interval before it drops a beat. Therefore, looking at the PR interval after asking the first two questions is the way to differentiate between Type I and II 2nd degree AV blocks.
While this method is sufficient for the majority of AV blocks, it is important to remember that there are always exceptions to the rule (for example, 2ː1, 3ː1, and 4ː1 AV blocks are 2nd degree AV blocks that have a regular rhythm).
1st Degree AV Block[edit | edit source]
Overviewː A first degree AV block is characterized by a regular rhythm with a prolonged PR interval (greater than 0.20 seconds). Remember that while the AV block is a finding, the underlying rhythm is sinus, therefore the correct name for the rhythm on the left is a sinus rhythm with a 1st degree AV block.
Rateː Generally 60-100, but may be any rate (e.g. a rate of 42 would be a sinus bradycardia with a 1st degree AV block.
Intervalsː Prolonged PR interval, all other intervals generally normal for rate.
Causesː AV nodal disease, enhanced vagal tone (e.g. athletes).
Treatmentsː None needed, this AV block is generally benign.
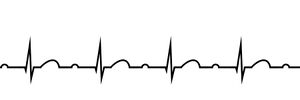
2nd Degree AV Block Type I (Wenckebach)[edit | edit source]

Overviewː The first of two 2nd degree AV blocks. This block is characterized by an increasingly prolonged PR interval which culminates in a dropped QRS complex. These dropped complexes are the reason there are more P waves than QRS complexes. Personally, the way I remember this block is that "one runs" (the p wave "runs" away from the QRS complex).
Rateː Regular until dropped complex occurs, irregular overall. Rate generally between 60 and 100 bpm, but may vary based upon patient presentation.
Intervalsː PR interval continually changes in a predictable way (always increases). All other intervals generally normal for rate (with the exception of an increased RR interval for the dropped beats).
Causesː Ischemia, increased vagal tone, myocarditis, post cardiac surgery, medication.
Treatmentsː If the patient is symptomatic, stable, and bradycardic atropine may have some effect but may also be ineffective due to decreased AV conduction. A fluid bolus may also be considered. If the patient is unstable, treat with TCP or vasopressors based upon presentation and other clinical indications.
2nd Degree AV Block Type II[edit | edit source]
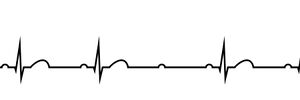
Overviewː The second of two 2nd degree AV blocks. This block is characterized by a normal PR interval with seemingly randomly dropped QRS complexes. These dropped complexes are the reason there are more P waves than QRS complexes.
Rateː Regular until dropped complex occurs, irregular overall. Rate generally between 60 and 100 bpm, but may vary based upon patient presentation.
Intervalsː All intervals generally normal for rate until dropped beat occurs, then RR interval increases for that beat.
Causesː Congenital heart disease, cardiomyopathy, myocardial ischemia/infarction, medications.
Treatmentsː If the patient is symptomatic, stable, and bradycardic atropine may have some effect but may also be ineffective due to decreased AV conduction. A fluid bolus may also be considered. If the patient is unstable, treat with TCP or vasopressors based upon presentation and other clinical indications.
3rd Degree AV Block[edit | edit source]
Overviewː 3rd degree AV blocks are different than all other AV blocks in several ways. First, there is no relationship between atrial and ventricular electrical activity (i.e. there is complete AV disassociation). Second, unlike all other AV blocks, the underlying rhythm is NOT a sinus rhythm, instead it will be a junctional or ventricular rhythm. For this reason, 3rd degree AV blocks tend to have a more bradycardic mechanical pulse despite normal or tachycardic atrial electrical activity. A third degree heart block can easily be a deadly rhythm and is often treated with TCP in the prehospital environment as atropine is unlikely to have any positive effect (atropine is an anticholinergic affecting the vagus nerve which innervates the atria primarily, because of the disconnect between atria and ventricles, atropine may increase atrial electrical activity while having no effect on ventricular rate). The distinction between a junctional and ventricular escape rhythm does not change any treatment decisions in the prehospital environment but can be helpful at localizing the location of the block.
Rateː Often bradycardic at the rate of the underlying escape rhythm (40-60 bpm for junctional, 20-40 bpm for ventricular).
Intervalsː Random PR interval, p waves often found "nested" in the QRS complex or T wave. Other intervals will vary but are generally normal for the underlying escape rhythm.
Causesː Myocardial ischemia/infarction, medication, pacemaker failure, severe heart disease.
Treatmentsː Do not delay TCP for administration of atropine. Atropine and vasopressors may be given IV/IO if line is present.
Other Rhythms and Abnormal Beats[edit | edit source]
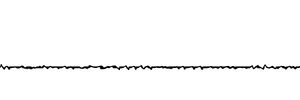
Asystole[edit | edit source]
Overviewː The stereotypical "flat line" that all medical shows use to show death. Asystole is a true cessation of any electrical activity in the heart. Because there is no electrical stimulus, there will be no mechanical contraction or pulse.
Rateː 0 bpm.
Intervalsː None.
Causesː Prolonged cardiac arrest, trauma, hypoxia.
Treatmentsː CPR and epinephrine. Depending on local protocol, the patient may be determined dead in the field if there is no change in rhythm/ROSC within a certain time period.
Premature Contractions (PAC, PJC, PVC)[edit | edit source]
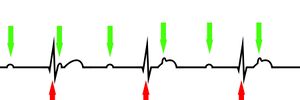
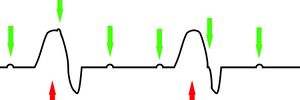
Premature contractions come in 3 flavors, each named after the location of the impulse that it originates from. All premature beats are so named because they occur prematurely, or before one would normally expect the next beat to occur. Premature atrial contractions (Figure 1) begin in the atria and thus have a p-wave with a linked QRS complex. Premature junctional contractions (Figure 2) begin in or just around the AV node and thus are narrow complex with a missing/flipped/retrograde p-wave. Premature ventricular contractions (Figure 3) begin in the ventricles and therefore are wide, abnormally shaped, and generally lack any discernible p-waves.
-
Figure 1. Sinus rhythm with a highlighted premature atrial contraction (PAC).
-
Figure 2. Sinus rhythm with a highlighted premature junctional contraction (PJC).
-
Figure 3. Sinus rhythm with a highlighted premature ventricular contraction (PVC).
Escape Beats[edit | edit source]
Escape beats are ectopic beats that can be classified as junctional or ventricular in origin. If there is a junctional or ventricular beat that does not come early (i.e. it is not a premature beat) then it may be classified as an escape beat, as it has helped your heart "escape" pulseless-ness.
Paced Beats[edit | edit source]
Pacemakers are becoming increasingly common, especially in the older populations. Not long ago, a pacemaker would look and feel like a pack of playing cards implanted in the patient's upper anterior chest, but newer pacemakers are much smaller and sleeker. Similarly, pacemakers used to produce large spikes just preceding an atrial or ventricular contraction on the ECG tracing that corresponded to the pacemaker firing; these spikes may not be visible with newer pacemakers. If the patient has a ventricularly paced rhythm, the beats generated will likely look more like a ventricular beat than a normally conducted beat; this is due to the ventricular pacemaker creating a ventricular beat. Note that normal p-waves may be found with seemingly ventricular beats if the patient has a dual chamber sequential pacemaker.
Documentation[edit | edit source]
Self Assessment[edit | edit source]
- Test your knowledge with this quiz.
Tips and Tricks[edit | edit source]
- Although QRS width is an important factor in determination of many different rhythms, there are outside factors that can affect QRS duration, such as bundle branch blocks, that can obscure the true rhythm. Therefore, for more complicated cases with high likelihood of outside factors and diseases, a 12 lead EKG may be helpful for true rhythm determination if it is difficult to figure out at first glance.
Additional Resources[edit | edit source]
- If you are interested in testing your rhythm interpretation skills in real-time, 6-Second ECG by Skillstat is a good, free way to practice.
- The website Life in the Fast Lane is a great resource that goes from shallow to deep knowledge for both rhythm analysis and 12 lead EKG interpretation.


