The aim of wound excision is to remove contaminating debris and all devitalised tissue. This should reduce both the bacterial burden and available substrate for microbial colonisation, resulting in fewer deep surgical site infections. In turn, this will lead to improved patient outcomes.
- Highly contaminated lower limb fractures should undergo immediate wound excision in theatre.
- Wound excision should be performed jointly by consultant orthopaedic and plastic surgeons
- High-energy lower limb fractures (likely Gustilo–Anderson Type IIIA and IIIB), which are not highly contaminated, should undergo wound excision within 12 hours of injury and all other lower limb fractures should be excised within 24 hours of injury. The consultant orthoplastic surgical team are best placed to determine the timing for individual patients based on clinical assessment
- Immediate surgical exploration is indicated in the presence of gross wound contamination, compartment syndrome, devascularised limb, or multiple injuries.
- Wound extensions are used to facilitate wound excision and allow inspection of deeper structures. In the tibia these should follow fasciotomy lines.
- Wound excision should be systematic to ensure all devitalised soft tissue and bone is removed whilst preserving the neurovascular bundles. Repeat wound excision may be required in the presence of tissues of doubtful viability whilst still respecting the timelines to reconstruction.
- Low-pressure lavage with a high volume of tepid 0.9% saline completes the wound excision.
Why Fasciocutaneous flaps?[edit | edit source]
Ensuring that blood vessels are safe for future local flap reconstruction is vital especially when fasciocutaneous flaps are used.
Fasciocutaneous tissue and muscle are both used for soft tissue coverage in the clinical setting, although the choice between them has been largely based on personal preference. Several authors of clinical studies state that muscle provides superior coverage of open tibial fractures.
Muscle flaps are said to provide excellent coverage for soft tissue defects over open tibial fractures. The plastic property of this tissue, conforming to the defect with elimination of dead space, may be important in reducing haematoma/seroma and subsequent infection. The perceived advantages of higher vasculature and resistance to infection have led to some authors preferring muscle to fasciocutaneous tissue.
Fasciocutaneous flaps have been used successfully in large clinical series to reconstruct open tibial defects. The advantages of simplicity, availability and versatility of local fasciocutaneous flaps, replacing ‘like with like’, offered significant advantages compared to complex microsurgical transfer and sacrifice of a muscle.
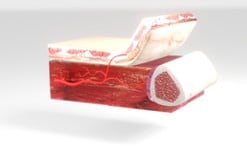
Fasciocutaneous flaps are tissue flaps that include skin, subcutaneous tissue and the underlying fascia. Including the deep fascia with its prefascial and subfascial plexus enhances the circulation of these flaps. They can be raised without skin and are then referred to as fascial flaps.
Fasciocutaneous flaps to used to provide coverage when a skin graft or random skin flap is insufficient for coverage (eg, in coverage over tendon or bones). The flap is oriented along the direction of the supplying vessel; knowledge of the direction or orientation of the fascial plexus, the fasciocutaneous perforators, and the fascial septum is required. They are simple to elevate, quick, and fairly reliable in healthy patients.
Because they are less bulky, fasciocutaneous flaps are indicated when thinner flaps are required. Unlike with muscle flaps, no functional loss occurs. Although these flaps provide a donor site in areas that are not available for random axial flaps, significant donor site morbidity can be associated with these flaps. Fasciocutaneous flaps are not as resistant to infection as muscle flaps. Monitoring flap failure occasionally can be difficult.
Anatomy[edit | edit source]
1. Fascio-cutaneous perforators (fasciocutaneous.html)
The following are the external landmarks of the vessels that are important to preserve so that flaps can be raised based on their perforators as in diagram 2
2. Classification (cormack.html)
Cormack and Lamberty classified fasciocutaneous flaps based on vascular anatomy.

- Type A is supplied by multiple fasciocutaneous perforators that enter at the base of the flap and extend throughout its longitudinal length. The flap can be based proximally, distally, or as an island.

- Type B has a single fasciocutaneous perforator, which is of moderate size and is fairly consistent. This flap may be isolated as an island flap or used as a free flap.

- Type C is based on multiple small perforators that run along a fascial septum. The supplying artery is included with the flap. It may be based proximally, distally, or as a free flap.
- Type D is an osteomyocutaneous flap, similar to Type C but including a portion of adjacent muscle and bone. It may be based proximally or distally on a pedicle or used as a free flap.
3. Lower Limb Fasciocutanous flaps (arteries.html)
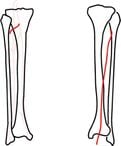
Anterior Tibial Artery Flap The anterior tibial artery flap is a Type B fasciocutaneous flap located on the anterolateral aspect of the leg between the knee and lateral malleolus. Based on the septocutaneous branches of the anterior tibial artery, it can measure 6 x 18 cm. The pedicle is 3 -4 cm in length and has a diameter of 0.3-0.8 mm. This flap most often is used for coverage of leg wounds around the tibia. It can be used as a sensory flap based on the superficial peroneal nerve. Most of the flaps of the leg can be designed as superiorly based, distally based, island, or turnover flaps.
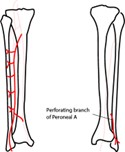
The Peroneal Artery Flap
The peroneal artery flap is a Type B fasciocutaneous flap based on the lateral leg over the fibula extending from the head of the fibula to the lateral malleolus. This flap can measure approximately 10 x 20 cm. Septocutaneous perforators of the peroneal artery supply its blood. The pedicle is 3 cm long and has a diameter of 0.5 mm. It can be used for coverage of defects of the middle and lower third of the leg. The superficial peroneal nerve may be included with a segment of fibula.
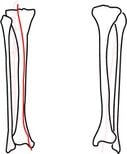
The Posterior Tibial Artery Flap
The posterior tibial artery flap is a Type B fasciocutaneous flap designed on the medial aspect of the leg from the knee to the medial malleolus. Based on septocutaneous perforators of the posterior tibial artery, it can be 6 x 18 cm. The pedicle is 2-4 cm long and has a diameter of 0.5-1 mm. It is used for coverage of defects of the middle and lower third of the leg and can include the saphenous nerve for sensory innervation.
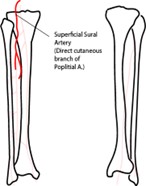
Sural Artery Flap
The sural artery flap is a Type A fasciocutaneous flap based on the sural artery direct cutaneous branch of the popliteal artery. The pedicle is 3 cm long and has a diameter of 1.4 mm. It is located between the popliteal fossa and the midposterior leg between the medial and lateral heads of the gastrocnemius muscle. The flap can measure 15 x 6 cm and may include the sural nerve as a neurosensory flap. Use this flap for wounds around the knee and upper leg.
Design[edit | edit source]
Transposition[edit | edit source]
The flap, which incorporates the Great Saphenous vein and Saphenous nerve, is rotated around a pivot 6cm from the tip of the medial malleolus where the distal most perforator is located.
Propeller[edit | edit source]
Defects distally can be closed by rotating the flap 180 degrees, pivoted about the perforator.




