This training module allows medical officers (non-specialist physicians) and general surgeons to become confident and competent in the gentle handling of delicate infant tissues as part of neonatal colostomy procedures performed in low to middle income countries (LMICs).
Overview[edit | edit source]
Global Impact[edit | edit source]
Nearly 2 billion infants and children globally lack access to safe, timely, and affordable surgical care.[1] Children account for over 40% of the population in sub Saharan Africa and 25-30% of the population in most LMICs. Performing surgery in this age group requires incredibly careful, gentle, and delicate handling of tissues to avoid complications and mortality. Handling neonatal tissue requires such psychomotor skills more than anywhere else and creating a safe colostomy for anorectal malformations - the leading congenital cause of intestinal obstruction in children in Africa - is the most typical example where such skills are required.[2]
In most of sub Saharan Africa and LMICs, there are very few pediatric surgeons and most neonates and children have no access to specialized care.[3] This means that surgery on children in most of these settings are performed by non-specialist physicians and general surgeons who have little or no training in the surgical care of children. Training these categories of staff in careful, gentle and delicate tissue handling would make it possible for them to perform emergency and essential surgical procedures in children in a safe manner, thereby, avoiding and minimizing complications and mortality.
The goal of this module is to make it possible for medical officers and general surgeons -- who are not specifically trained as pediatric surgeons -- to be able to provide the needed surgical care for nearly 2 billion infants and children around the world. This module teaches gentle tissue handling skills that are transferable to other life-saving surgeries in newborns and children. These can include but are not limited to the following essential surgical procedures identified by the World Bankː
- colostomy creation for anorectal malformations
- surgical management of Hirschsprung’s Disease, and
- repair of typhoid ileal perforations.[4]
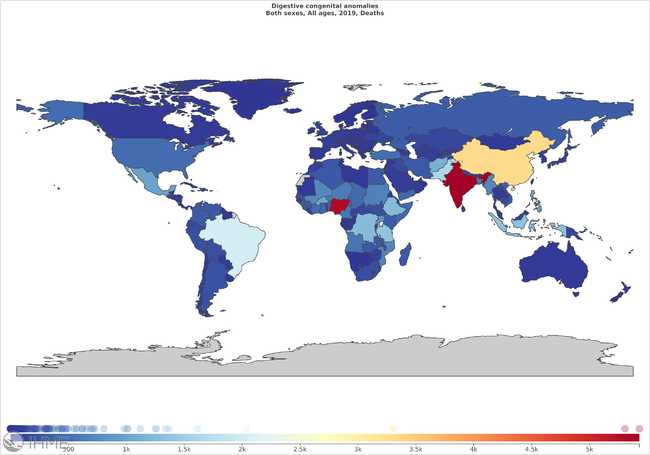
In 2017, an estimated 14.3 million cases of typhoid and paratyphoid fevers occurred globally, resulting in 135,900 deaths.[5] In sub-Saharan Africa, there were an estimated 1,729,900 cases of typhoid and paratyphoid fevers in 2017. The method of transmission is through faeco-oral ingestion and many children are infected because of their unguided eating habits. The sequelae of untreated typhoid and paratyphoid infections include: altered mental status, ileus, gastrointestinal bleeding, bowel perforation, sepsis, and death. In 2019, the global prevalence and incidence of digestive congenital anomalies was 2,897,550 and 769,584 cases with 47,332 deaths.[6]
Frugal Simulators for Psychomotor Skills Training[edit | edit source]
The specific psychomotor skills that this module teaches are:
- Gentle and delicate tissue handling
- Avoiding crushing tissue
- Avoiding undue tension and pull
- Avoiding tight sutures
This module provides a previously used cigarette model to teach learners to avoid undue tension and compression and creating sutures that are too tight when performing an enterocutaneous anastomosis in a newborn.
This low-tech Neonatal Enterocutaneous Anastomosis Simulator is made from inexpensive materials that are readily available within the intended place of use.
Low-cost simulators are often improvised out of locally available materials in LMICs but these simulators lack objective data to validate that the user's learnings will directly translate into the safe, clinical performance of that psychomotor skill and not foster the development of anti-skills. We will be addressing the shortcomings of our inexpensive, low-tech simulator in teaching the performance of gentle tissue handling skills by using live animal models to evaluate whether the simulator is effective in training.
The cigarette model costs 5-10¢ USD and simulates the fragile, delicate tissues of a neonate. Although the cigarette suturing activity simulates a bowel anastomosis, the gentle tissue handling skills are the same for performing an enterocutaneous anastomosis in a newborn. The user's learnings from this cigarette suturing activity will directly translate into the clinical performance of the enterocutaneous anastomosis for a colostomy in a newborn.
Each Neonatal Enterocutaneous Anastomosis Simulator (consisting of two cigarettes) can accommodate about four sutures. However, an average of 8-12 sutures are placed in the enterocutaneous anastomosis step during colostomy creation in a newborn. To overcome this shortcoming of this frugal simulator in teaching the performance of gentle tissue handling skills, the module's self-assessment framework requires that the learner must successfully complete a minimum of 12 consecutive sutures on a total of 3 pairs of cigarettes.
The user's learnings from this simulator will directly translate into the clinical performance of gentle tissue handling skills for a colostomy in a newborn.
Syllabus[edit | edit source]
The learner should study the content of knowledge pages 1-2 and then take the readiness test. It is highly recommended that the learner be familiar with this content before proceeding to the skill pages.
Phase 1: Knowledge Review[edit | edit source]
- Protocol for Management of a Neonate Requiring a Colostomy
- Descending Colostomy with Separated Stomas
- Colostomy in Newborns Self-Administered Readiness Test
Phase 2: Simulator Build[edit | edit source]
Phase 3ː Skills Training[edit | edit source]
Phase 4ː Self-Assessment[edit | edit source]
Overview[edit | edit source]
The Neonatal Enterocutaneous Anastomosis Simulator allows the user to self-generate targeted feedback which enables the user to verify they are practicing the appropriate gentle tissue handling skills; modify their performance to improve competence (if required); and determine when they have practiced to a sufficient level of mastery to perform a colostomy in a newborn.
This module's self-assessment framework will include a:
- Checklist review for the basic, intermediate, advanced, and (optional) expert gentle tissue handling skills training
- Visual inspection and photographing of suturing performance on the Neonatal Enterocutaneous Anastomosis Simulator
- Training Logbook to record suturing performance and training dates
Checklist[edit | edit source]
The checklist for the Neonatal Enterocutaneous Anastomosis Simulator is outlined belowː
- Cigarettes ends are successfully sutured
- No spilling of the contents of the cigarettes
- No tears on the cigarette wrap
- Ends not rumpled or squashed
Visual Inspection[edit | edit source]
The learner will conduct a visual inspection with the checklist and use a cellphone camera to photograph their suturing performance on the Pediatric Bowel Anastomosis simulator:
- to verify completion of the Neonatal Enterocutaneous Anastomosis Simulator training and self-assessment framework
- for potential remote evaluation and feedback by a pediatric surgeon to independently confirm that the learner has practiced to a sufficient level of mastery to perform the procedure in a patient.
Training Logbook[edit | edit source]
The learner will use the Training Logbook to:
- set training goals
- check suturing performance
- record task completion dates, and
- track skills progression over time.
The Training Logbook records the learner's suturing performance to enable the user to ensure they are practicing the appropriate gentle tissue handling skills; modify their performance to improve competence; and determine when they have practiced to a sufficient level of mastery to perform the procedure in a patient.
When the learner has successfully completed a minimum of 12 consecutive sutures on the dry lighting ends on a total of 3 pairs of cigarettes (advanced skills training), then they will have practiced to a sufficient level of mastery to perform the procedure in a patient.
Innovation and Scaling Adoption[edit | edit source]
Innovation[edit | edit source]
Surgical simulation training is primarily focused on adult patients and not customized to neonatal patients with congenital anomalies.[7] This module is designed to reach and support as many medical officers and general surgeons in LMICs as possible and enable pediatric surgical skills acquisition outside of training centers.
Self-Assessed Training[edit | edit source]
This simulation-based training module does not require access to teachers, cadavers, animal models or expensive mannequins. The simulator is built from locally available, low-cost materials and allows users to self-generate targeted feedback to verify they are practicing the appropriate gentle tissue handling skills; modify their performance to improve competence; and determine when they have practiced to a sufficient level of mastery to perform a colostomy in a newborn.
Low Cost[edit | edit source]
This module offers significant value for money in comparison to existing approaches for pediatric surgical simulation training. The most commonly used surgical simulation training models for newborns are live, anesthetized animals, such as very small rabbits, piglets, or baby goats. We calculated the total anesthesia, staffing, and consumable material costs (excluding sutures) per live animal model in Nigeria is $368.81 USD. The total known material costs (excluding sutures) of the Neonatal Enterocutaneous Anastomosis Simulator in Nigeria is between 5¢ to 10¢ USD. The learner also saves on the costs of course fees, travel, lodging, and missing work.
Evaluation[edit | edit source]
On September 29, 2021, the gentle tissue handling skills training module with basic, intermediate, advanced and optional expert training levels was tested by five medical officers recruited at the National Hospital of Abuja in Nigeria. Two live animal models (rabbits anesthetized with ketamine) were deployed. All five medical officers were able to achieve technical proficiency to the advanced skills training level. Three medical officers were able to achieve technical proficiency to the optional expert skills training level on their own. Two of the latter three medical officers were able to successfully complete the procedure on the live animal models. This preliminary user testing indicates that demonstrating technical proficiency to the advanced training level is achievable in our target learners and translates into safe procedural skills in live animal models. This confirmed our decision to maintain our skills training module with basic, intermediate, advanced and optional expert skills training levels.
On August 8, 2021, we trialed the NASA Task Load Index for users of the module but observed that the survey's generic questions did not provide useful, targeted feedback to the learner above and beyond this module's existing self-assessment framework, and that learner compliance with completing the forms was poor. We opted to remove the NASA Task Load Index from our self-assessment framework because it did not add any additional training value to the learner and this would reduce the administrative burden on the learner.
Design for Extreme Accessibility in Low Resource Settings[edit | edit source]
This module applies user-centered, reproducible, and accessible design choices to maximize adoption in resource-constrained settings.
User-Centered Design[edit | edit source]
Medical officers are fully trained physicians who have not undergone any additional formal surgical training. Nevertheless, they are required to perform or are performing surgical procedures in children in LMICs due to severe shortages of pediatric surgeons. General surgeons have undergone formal advanced training in the surgical care of adults but have not been trained to perform surgery on children. They are currently involved in providing surgical care for children in LMICs due to severe shortages of pediatric surgeons.
The Global Initiative for Children's Surgery (GICS) has already engaged with these medical officers and general surgeons and created the Optimal Resources for Children's Surgery[8] which carefully lays out the skills required by these personnel to perform surgical procedures in children.[9] This module addresses user needs by teaching learners the preparation of a newborn for surgery, surgical decision-making in infants, gentle tissue handling as well as postoperative care following surgery in neonates to ensure a safe outcome.
We conducted a survey of 16 pediatric surgeons around the world through the Global Initiative for Children's Surgery (GICS) to identify the key psychomotor skills required to safely perform colostomy in the newborn and the ideal features of a neonatal stoma.
Reproducible Design[edit | edit source]
The frugal Neonatal Enterocutaneous Anastomosis Simulator is made from locally available and inexpensive materials and is designed to be fully reproducible in the intended place of use.
No tools, specialized equipment, or technical expertise is required to construct the Neonatal Enterocutaneous Anastomosis Simulator.
When possible, the equipment is reusable to minimize the use of consumables and maximize its lifespan in the place of use.
This module will offer value for money in comparison to existing approaches. Each Neonatal Enterocutaneous Anastomosis Simulator, which consists of 2 cigarettes, costs between 5¢ to 10¢ USD. In Nigeria, the retail cost of 1 packet of Pall Mall cigarettes is 400 ₦.[10] Each packet contains 20 sticks of cigarettes. Thus, an individual cigarette stick costs 20 ₦ (400 ₦/20 sticks) at retail pricing which is equal to about 5¢ USD per cigarette. In Nigeria, the wholesale cost of 1 packet of Pall Mall cigarettes is 210 ₦. Each packet contains 20 sticks of cigarettes. An individual cigarette stick costs 10.5 ₦ (210 ₦/20 sticks) at wholesale pricing which is equal to about 2.5¢ USD.
Although 4-0 or 5-0 Vicryl or PDS sutures with a round bodied needle should be used during a colostomy procedure on neonates; this module recommends using inexpensive 4-0 or 5-0 silk sutures with a round bodied needle for skills training to maximize affordability and accessibility for learners.
Accessible Design[edit | edit source]
This Appropedia-based module (including the Training Logbook) is available in the 6 official languages of the United Nations and other languages to help ensure that surgical practitioners from anywhere in the world will be able to engage with the content without barriers or gatekeeping.
This module does not require the downloading of a mobile app, creation of an account, inputting of a username and password, or paying journal or other subscription fees to access the training content.
Offline and Off Grid Access[edit | edit source]
Self-directed training is typically only available online or via mobile apps. These traditional approaches have accessibility barriers in low resource settings because:
- Over 4 billion people do not have access to the Internet.[11]
- The penetration of high-speed Internet connectivity (broadband, 3G, or better mobile connections) is less than 30% in rural regions.[12]
- Smartphones only make up 50% of total connections in sub Saharan Africa.[13]
- An estimated 770 million people worldwide lack access to electricity and 600 million of these individuals reside in sub Saharan Africa.[14]
The demand for this module will be greatest in regions with little or no access to the Internet, smartphones, or grid electricity. When possible, we have made as much of the module content (including step-by-step simulator build, simulator use, and self-assessment framework instructions with photos instead of only videos) available in pdf format using Appropedia's export function for offline access. Paper-based versions of surgical training modules are inadequate because they cannot provide video and digital interactive content which is essential for surgical skills training and self-assessment frameworks.
Over 235 million people require humanitarian assistance[15] and 44.7 million people in conflict zones are unable to access essential surgical care.[16] Every day, hospitals, patients, healthcare staff, ambulances, and aid workers come under attack in regions affected by conflict and other emergencies.[17][18] Online platforms and mobile phones are vulnerable to security breaches which can be used to target bombing attacks on hospitals in conflict zones.[19] It is critical that this training module be available offline to remain isolated from any surveillance from an external Internet connection to prevent hackers from targeting healthcare workers and facilities in conflict zones.
We use Linux open-source software and an offline (air gapped), energy-efficient, ultraportable Raspberry Pi with integrated 7-inch touchscreen display to make this module safely available to the surgical practitioners serving the 4 billion people who do not have access to the Internet and the millions of the most vulnerable civilians in conflict zones.
A 2015 study shows that a Raspberry Pi ($35 USD) with a 10 inch display consumes almost the same amount of energy (21.24 kJ/h) as a smartphone ($400 USD) with 4.7 inch display (18 kJ/h), 4.2 times less energy than a $320 USD tablet (90 kJ/h), and 8.5 times less energy than a $728 USD laptop (180 kJ/h).[20] The advantages of using a Raspberry Pi with an integrated 7-inch display screen over a smartphone or tablet are reduced costs, energy efficiency and a larger screen area to optimize learning.
To minimize the use of storage capacity offline and maximize the number of validated, open-source GSTC Appropedia modules that can be stored and made available offline on a Raspberry Pi, we designed this module to minimize the number of secondary or tertiary links, when possible. Our team will be recruiting volunteer Medical Makers to help make GSTC Appropedia modules available offline to maximize the global impact of the GSTC.
Last Mile Implementation[edit | edit source]
We will be evaluating the concept of setting up a Medical Makerspace in a government hospital in a LMIC to serve as a training, manufacturing, and distribution center that educates local Makers to make GSTC simulation training modules available offline at the lowest cost for practitioners in remote or rural areas across the country. We have developed a partnership to deliver this offline GSTC module on demand to up to 33,000 general hospitals and 16 tertiary hospitals across Nigeria that do not have access to a pediatric surgeon.[21]
The offline version of this training module can be transported anywhere in Nigeria by motorbikes within 1-2 days[21] and delivered up to 80 km away on demand via fixed wing drones in Nigeria's Kaduna state.[22] The offline version of this training module is designed to comply with cargo weight and size requirements for medical delivery drones that are already operating in Nigeria, Rwanda, Ghana, India, Philippines, and the United States.
References[edit | edit source]
- ↑ Mullapudi B, Grabski D, Ameh EA, Ozgediz D, Thangarajah H, Kling K, Alkire B, Mearae JG, Bickler S. Estimates of number of children and adolescents without access to surgical care, Bull World Health Organ 2019;97:254–258. DOI: https://doi.org/10.2471/BLT.18.216028
- ↑ Lawal TA. Overview of Anorectal Malformations in Africa. Front. Surg. 2019 Mar;6:7. DOI: https://doi.org/10.3389/fsurg.2019.00007
- ↑ Sanjay Krishnaswami, Benedict C. Nwomeh, Emmanuel A. Ameh, The pediatric surgery workforce in low- and middle-income countries: problems and priorities, Seminars in Pediatric Surgery. Volume 25, Issue 1, 2016, Pages 32-42, ISSN 1055-8586, https://doi.org/10.1053/j.sempedsurg.2015.09.007.
- ↑ Debas, H. T., P. Donkor, A. Gawande, D. T. Jamison, M. E. Kruk, and C. N. Mock, editors. 2015. Essential Surgery. Disease Control Priorities, third edition, volume 1. Washington, DC: World Bank. doi:10.1596/978-1-4648 -0346-8. License: Creative Commons Attribution CC BY 3.0 IGO.
- ↑ GBD 2017 Typhoid and Paratyphoid Collaborators. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis. 2019 Apr;19(4):369-381. doi: 10.1016/S1473-3099(18)30685-6. Epub 2019 Feb 18. PMID: 30792131; PMCID: PMC6437314.
- ↑ Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020. Available from http://ghdx.healthdata.org/gbd-results-tool.
- ↑ Dr. Shant Shekherdimian. Personal communication. MIT Solveathon - Eastern Europe + Middle East & North Africa, September 19, 2020.
- ↑ Grabski, D., Ameh, E., Ozgediz, D. et al. Optimal Resources for Children's Surgical Care: Executive Summary. World J Surg. 2019 Apr;43(4):978–980. DOI: https://doi.org/10.1007/s00268-018-04888-7.
- ↑ Goodman LF, St-Louis E, Yousef Y, Cheung M, Ure B, Ozgediz D, Ameh EA, Bickler S, Poenaru D, Oldham K, Farmer D, Lakhoo K; GICS Collaborators. The Global Initiative for Children's Surgery: Optimal Resources for Improving Care. Eur J Pediatr Surg. 2018 Feb;28(1):51-59. DOI: https://doi.org/10.1055/s-0037-1604399.
- ↑ Dr. Chisom Udeigwe-Okeke. Personal communication. October 4, 2021.
- ↑ Internet for All: A Framework for Accelerating Internet Access and Adoption (White Paper). World Economic Forum, 12 May 2016. URL: https://www.weforum.org/reports/internet-for all-a-framework-for-accelerating-internet-access-and-adoption.
- ↑ International Telecommunication Union (ITU), 2015, ICT Facts & Figures URL: https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2015.pdf.
- ↑ The Mobile Economy: Sub-Saharan Africa 2020. GSM Association. URL: https://www.gsma.com/mobileeconomy/wp-content/uploads/2020/09/GSMA_MobileEconomy2020_SSA_Eng.pdf.
- ↑ IEA (2018), Population without access to electricity falls below 1 billion, IEA, Paris https://www.iea.org/commentaries/population-without-access-to-electricity-falls-below-1- billion.
- ↑ United Nations Office for the Coordination of Humanitarian Affairs. Global Humanitarian Overview 2021. [Internet]. Geneva (Switzerland): United Nations Office for the Coordination of Humanitarian Affairs; 25 November 2020 [cited 2021 Aug 17]. Available from: https://gho.unocha.org/.
- ↑ Creating Hope in Conflict: A Humanitarian Grand Challenge - Request for Proposals February 19, 2018.
- ↑ International Committee of the Red Cross. Why we can't save her life | On The Frontline. [Internet]. San Bruno (CA): Youtube; 2018 May 3 [cited 2021 Aug 27]. Available from: https://www.youtube.com/watch?v=wm0TYebjyHQ.
- ↑ International Red Cross and Red Crescent Movement. HCID Initiative: A global initiative. [Internet]. Geneva (Switzerland): International Red Cross and Red Crescent Movement; 2018 [cited 2021 Aug 27]. Available from: https://healthcareindanger.org/hcid-project/
- ↑ Fish I. My computer was hacked so Russian warplanes could bomb underground hospital in Syria, claims surgeon who carried out remote surgery in Aleppo. [Internet]. London (UK): The Daily Mail; 2018 March 21 [revised 2018 Mar 21; cited 2021 Aug 17]. Available from: https://www.dailymail.co.uk/news/article-5525391/British-surgeons-computer-hacked-Syrian-hospital.html.
- ↑ Anwaar W, Shah MA. Energy Efficient Computing: A Comparison of Raspberry PI with Modern Devices. International Journal of Computer and Information Technology. 2015 Mar;4(2):410-413.
- ↑ 21.0 21.1 Riders for Health. Medical supply chain logistics. [Internet]. Olney (MD): Riders for Health II; 2021 [cited 2021 Aug 17]. Available from:https://www.riders.org/how-we-work/services/distribution-of-pharmaceuticals-and-medical-supplies/.
- ↑ George L. Nigeria's Kaduna pairs with Zipline for drone-delivered COVID vaccines. [Internet]. Lagos (Nigeria): Reuters; 2021 Feb 3 [cited 2021 Aug 18]. Available from: https://www.reuters.com/article/uk-health-coronavirus-nigeria-drones/nigerias-kaduna-pairs-with-zipline-for-drone-delivered-covid-vaccines-idUSKBN2A31MM.