This page is part of the paramedic curriculum and is currently under development. Content will be added to this page, but there is no public knowledge currently available from this page. We thank you for you for your visit and hope you return when this program has been completed. Should you be interested in the foundation of all basic paramedic skills, click here to return to the EMT NREMT Skillset home page. For other sustainable projects, see Appropedia's home page.
This page is intended as a supplementary resource to the didactic knowledge found in a paramedic program. This will cover the basic anatomy and physiology of needle decompression. This page will give basic guidelines and information on needle decompression without bias towards a single device or manufacturer. Always refer to local protocols when using a new or unfamiliar monitor/defibrillator. If you are on this page to learn the sequence of events to perform a needle decompression, skip to Performing the Decompression.
What is needle decompression?[edit | edit source]
Needle decompression, also known as needle thoracostomy, is the procedure in which a needle is inserted into a patient’s chest with the intent of relieving a suspected or confirmed tension pneumothorax.
Why do we decompress?[edit | edit source]
Needle decompression allows for the release of trapped air from the affected side of a tension pneumothorax, thereby allowing for re-expansion of the lung and a decrease in pressure on the heart and its surrounding vasculature.
Pneumothorax and sucking chest wound[edit | edit source]
A sucking chest wound is created when a patient sustains a penetrating injury that breaches the chest wall and creates an opening greater than 1/3 the diameter of the trachea. As the patient attempts to breathe and their diaphragm contracts, air is drawn in through this opening. Sucking chest wounds are commonly treated with occlusive dressings or chest seals with one-way valves.
A pneumothorax by definition is air within the thorax, specifically air that is outside of the lung space. Pneumothoraxes come in several varieties: simple pneumothorax, traumatic pneumothorax, and tension pneumothorax.
Simple pneumothorax[edit | edit source]
[Simple Pneumothorax Image] (Fig 1)
A simple, or spontaneous, pneumothorax (Figure 1) is a condition in which abnormalities and weaknesses in the lung parenchyma undergo a rupture which allows air from the lung to enter the of the thoracic cavity. Patients who are tall and thin tend to have higher incidences of spontaneous pneumothorax, which may occur while undergoing strenuous activity. Patients with simple pneumothoraxes rarely progress to tension pneumothorax and are generally not able to be treated by EMS providers with a needle decompression.
Traumatic pneumothorax[edit | edit source]
[Traumatic Pneumothorax image] (Fig 2)
A traumatic pneumothorax (Figure 2) forms from the progression of a sucking chest wound or from trauma to the lung tissue itself. A traumatic pneumothorax may progress to a tension pneumothorax and as such should be treated by EMS to prevent worsening of the patient’s condition. A traumatic pneumothorax with no signs of tension pneumothorax should be treated with an occlusive dressing or chest seal with one-way valve.
Hemo- vs pneumo- (thorax) (Fig 3)[edit | edit source]
[Hemothorax image]
A hemothorax (Figure 3) is a condition in which blood, instead of air, enters the thoracic cavity. This can occur after a traumatic event and can cause the same complications as a pneumothorax.
Tension pneumothorax (Fig 4)[edit | edit source]
[Tension Pneumothorax image]
A tension pneumothorax (Figure 4) is characterized by significant pressure intrapleural on a collapsed lung which forces that lung against the heart and great vessels. This type of pneumothorax is a life threat as it can easily cause obstructive shock by impeding normal cardiac function and/or venous return. A tension pneumothorax may be treated by needle decompression. Patients with a tension pneumothorax may present with shortness of breath, tachycardia, hypotension and unilateral lung sounds among other findings. A late sign of tension pneumothorax is a deviation of the trachea to the opposite side of the affected lung.
Anatomy of decompression[edit | edit source]
Location[edit | edit source]
There are two locations where a pleural decompression is commonly performed in the emergency setting: the anterior and the midaxillary. Either location may be used if allowed by local protocol and patient presentation, and each has a reason why it may be utilized as opposed to the other.
Anterior (2nd intercostal space)[edit | edit source]
The anterior approach is indicated as a first-line treatment by some EMS agencies as it leaves the midaxillary region free for a tube thoracostomy (chest tube) to be placed. When utilizing the anterior approach, the needle is advanced through the 2nd intercostal space on the midclavicular line, the location of which is shown in Figure 5). Remember, midclavicular is not halfway across the chest from the midline; instead it is halfway along the clavicle and is therefore more lateral than one may expect (some sources use the nipple line as an approximation of the midclavicular line).
[Image Anterior Decompression] (Fig 5)
Midaxillary (4th or 5th intercostal space)[edit | edit source]
The midaxillary approach is indicated as a first line treatment by some EMS agencies. Through the 4th or 5th intercostal space on the midaxillary line
[Image Lateral Decompression] (Fig 6)
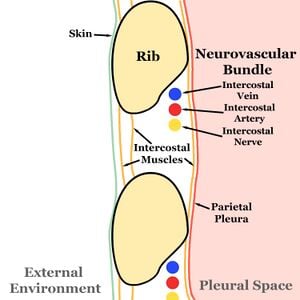
The Neurovascular Bundle[edit | edit source]
Performing the Decompression[edit | edit source]
To perform a needle thoracostomy (needle decompression), the provider must utilize a large bore (preferably 16 g or larger for a standard adult patient) catheter-over-needle system. Commercial devices do exist, if using a commercial device, follow the manufacturer’s instructions.
Items needed[edit | edit source]
- Catheter-over needle system of the correct gauge and length (most commercial devices are 14 g and 3.25" with no flash chamber)
- Skin preparation (alcohol, betadine, chlorhexidine)
- Sharps container
- One way valve to prevent reentry of air (best practice)
- Syringe (with or without saline) (optional and useful in loud environments to visualize entry into the pleural cavity)
Procedure[edit | edit source]
After identifying a tension pneumo/hemothorax and deciding to perform a needle decompression:
- Gather all materials and explain procedure to patient if time and patient condition permits.
- Identify landmarks and puncture site.
- Clean puncture site with aseptic technique, ideally with chlorhexidine.
- Enter chest wall at selected location with the needle at a 90° angle to the chest wall. Enter the chest wall lower in the intercostal space to avoid damaging the neurovascular bundle (Figures 8a and 8b).
- Advance needle until a hiss or "whoosh" of air is heard, indicating entry into the pleural cavity. If using a syringe, partially fluid filled or empty, continuously aspirate and advance needle through chest wall until resistance to aspiration disappears/bubbles are visualized which indicates entry into the pleural cavity (Figure 8c).
- Stop advancement of the needle to minimize possibility of damage to thoracic structures and advance catheter over needle into the pleural space (Figure 8d).
- After catheter is fully advanced, remove needle from catheter and dispose in appropriate sharps container (Figure 8e).
- If utilizing one-way valve device, attach to patient's skin or catheter hub as directed by local protocol or manufacturer recommendation.
-
Figure 8a. Approach the chest wall with the needle and catheter system at a 90° angle.
-
Figure 8b. Continue to advance needle and catheter system through chest wall, continuously aspirating if a syringe is attached.
-
Figure 8c. Hiss of air, lack of resistance to aspiration, or visualization of bubbles in the syringe as needle tip enters pleural cavity.
-
Figure 8d. Catheter is advanced into pleural cavity while needle is not moved.
-
Figure 8e. Needle removed from catheter after catheter has been fully inserted.
Documentation[edit | edit source]
- "Patient found complaining of severe SOB and chest pain following GSW to the left anterior chest with exit wound to the posterior. Patient assessment reveals absent left-sided breath sounds, right sided tracheal deviation, JVD. Patient hypotensive and tachycardic with SPO2 82% on room air. Pleural decompression performed at the midaxillary line (2nd ICS) with 14 g 3.25" catheter to return of left-sided breath sounds (diminished), relief of hypotension, and mild relief of SOB. Conventional chest seal placed over catheter."