CPR with AED is included in this California-based EMT program as it is required for National NREMT registration and skills verification for California Registration. This page is for Infant CPR, there are separate pages for adult and child.
Cardiopulmonary Resuscitation (CPR) is a series of immediate actions to take to restore the flow of oxygenated blood to a person's brain and organs when they suffer Sudden Cardiac Arrest (SCA). If the flow of oxygenated blood to the brain is not restored within a few minutes the victim could die or suffer irreversible brain damage.
CPR[edit | edit source]
For the purpose of CPR an infant is defined as from birth to 1 year of age.
Single Rescuer (Witnessed vs Unwitnessed)
- Check that the area is safe for you and your patient, and don appropriate PPE (PENMAN)
- Check for alertness/responsiveness by flicking the sole of the foot (AVPU)
- Activate the 911 system via cell phone if available-(If arrest was unwitnessed, you are alone and you do not have a cellphone perform 2 minutes of CPR before leaving the patient to activate 911 and retrieve an AED, if available)
- Place the person on their back on a hard surface
- Open their airway with a head tilt to slightly lift the chin
- Simultaneously assess for brachial pulse and breathing for no more than 10 seconds
- If the arrest was witnessed you may leave to activate 911 if not already done and to retrieve an AED. If the arrest was not witnessed immediately proceed to the next step.
- If patient is unresponsive and is not breathing or has abnormal breathing (ie. Agonal breathing) and no definitive pulse was felt, or the pulse was 60 beats per minute or less (one second or more between beats) immediately begin chest compressions of >1/3 anteroposterior depth of the chest (about 1.5 inches) at a rate of 100-120, allowing for full chest recoil. (See Self-Assessment sidebar for additional information)
- After performing 30 compressions administer two (2) rescue breaths via BVM, mouth to mouth, mouth to mask or through stoma as appropriate. (avoid excessive ventilation)
- After the two rescue breaths have been administered immediately resume chest compressions.
- If the arrest was unwitnessed and you are still alone after 5 cycles of 30 compressions and two breaths you may leave the patient to activate the 911 system (if not already done) and to retrieve an AED.
- Repeat the cycles of 30 chest compressions and two rescue breaths and use the AED/Defibrillator as soon as it is available. (When two rescuers are available provide cycles of 15 compressions and two breaths). Continue cycles of compressions and ventilations until properly relieved by rescue personnel.
If additional personnel are available switch compressors approximately every 10 cycles of 15 compressions and two breaths (approximately 2 minutes) to prevent exhaustion.
AED[edit | edit source]
An AED should be applied as soon as it is available. The AED should be applied while CPR is ongoing. There are many variants of AED’s in use, however, they all follow four universal steps with slight variations on how each step is performed.
The Four Universal Steps to operating an AED are:
- Turn the machine on
- Apply pads to patients bare chest
- Analyze the heart rhythm
- Deliver a shock if advised by the AED
Detailed description of the Four Universal Steps to operating an AED:
1. Turn the Machine On: this step is usually accomplished by either pushing the button labeled “On” or by opening the lid. (Once the machine is on it will verbally prompt the steps of operating the AED)
2. Apply Pads to Patients bare chest: place the pads as depicted on the pads or packaging. (See Sidebar for special circumstances such as medication patches, wet skin, hairy chest, jewelry, etc..)
- Analyze the heart rhythm: this step is usually accomplished in one of three ways. On many AED's the pads are already connected to the machine and placement the second pad on the patient’s chest completes a circuit that will being the analyze process, on some AED's the pads are not connected to the machine plug them in now and the machine will start the analyze process and finally some machines require the operator to physical push a button labeled “Analyze” to start the analyze process. Follow voice prompts if unsure. (Important: Ensure that no one is touching the patient while the machine is analyzing the heart rhythm)
4. Deliver a shock if advised to by the AED: Once the analyze process is complete the machine will either state “Shock advised” or “No shock advised”. If the machine determines that no shock is advised immediately begin CPR starting with chest compression. If the machine determines that a shock is advised it will begin to charge the machine to the proper energy setting (it is appropriate to perform compressions while the machine is charging). Once the machine is charged there are two ways to deliver the shock depending upon the type of AED in use. In either case verbally and visually ensure that everyone is clear of the patient (No one touching the patient) by loudly stating “Clear!” prior to the shock being delivered.
- A semi-automatic machine requires you to physically push the “Shock” button which will be flashing once the machine is sufficiently charged, the voice command will be advising people to stay clear.
- A fully automatic machine will deliver the shock automatically and will begin a countdown to when the shock will be delivered, it will also be advising people to stand clear of the patient. Regardless of the type of AED used once the shock has been delivered immediately begin CPR beginning with chest compressions. Every two minutes the AED will advise people to stand clear so that it can begin the analyze process and will then again advise “Shock Advised” or No Shock Advised’. Unless the patient is moving and showing signs of life, anytime the machine states “No Shock Advised” immediately begin CPR. If the machine determines a shock is advised repeat the process of clearing the patient, delivering the shock and starting CPR.
(Note: Once the machine is turned on voice commands will walk the rescuer thru the steps of operating that particular AED, being familiar with these steps beforehand results in faster application of the AED and a more efficient rescue attempt.)
Running the Pediatric Cardiac Arrest[edit | edit source]
An AED can be used on children and infants and should be used as early as possible for the best chance of improving survival. Check the AED when it arrives at the scene. Pediatric pads should be used if the person is less than eight years old. Standard (adult) pads may be used if pediatric pads are not available. If using standard (adult) pads, do not let the pads touch. For infants less than a year old, a manual defibrillator should be used if available. If a manual defibrillator is not available, an AED may be used. Some AEDs have a switch that can be set to deliver a pediatric shock. If available, turn the switch on when using on children younger than eight years old. If the AED cannot deliver a pediatric shock, an adult shock should be given. It is important to remember an electric shock may be the cure for a fatal heart rhythm.
AED STEPS FOR CHILDREN AND INFANTS
Retrieve the AED .
- Open the case.
- Turn on the AED. Expose the person's chest If wet, dry the chest.and remove any medication patches.
- Open the Pediatric AED pads and peel off the backing.
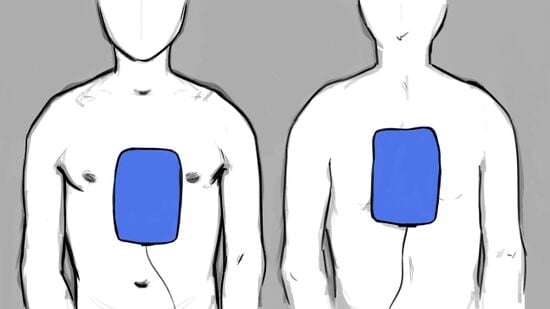
- Apply one pad on the upper right chest above the breast. For infants, apply on upper left chest
- Apply the second pad on lower left chest below the armpit. For infants, apply second pad to back
- Ensure wires are attached to the AED box
- Stop CPR and instruct others not to touch the child.
- Let AED analyzes the rhythm.
- If AED message reads "Shock," then either wait for the AED to deliver the shock (fully automatic versions) or press and hold flashing shock button until shock is delivered.
10. Resume CPR for two minutes
11. Repeat steps 7-10.
Troubleshooting: If AED message reads "Check Electrodes," then ensure electrodes make good contact and are firmly plugged into the AED box.
Documentation[edit | edit source]
Documentation of the CPR intervention should be included in the Patient Care Report (PCR). For a cardiac event ensure the following are included:
- Patient data: age, gender, and any comorbid conditions.
- Event data: was collapse witnessed or unwitnessed, location of event, time from collapse to the beginning of cardiopulmonary resuscitation (CPR) if known.
- Observations and interventions: initial rhythm if known, essential interventions (how long CPR was performed, AED application, number of shocks delivered) with times recorded. Note time from collapse to first defibrillation when the initial rhythm is ventricular fibrillation or pulseless ventricular tachycardia.
- Outcomes: return of spontaneous circulation (for at least 20 minutes), transport, or discontinuation of CPR
Self Assessment[edit | edit source]
- Test your knowledge using this quiz.
Tips and Tricks[edit | edit source]
- The four universal steps to operating an AED are: ON-PADS-ANALYZE-SHOCK (if advised.)
- Perform CPR on an infant or child who is showing signs of poor perfusion (i.e. altered level of consciousness, poor skin signs) with a heart rate of 60 beats per minute or less. The EMS adage for infants and children is-"60 or less better compress"
- For a single rescuer the compression to ventilation ratio is 30 compression to 2 breaths for all ages, when there are two rescuers the compression to ventilation ratio becomes 15 compressions to 2 breaths for Infants and Children and remains 30 compression to 2 breaths for adults.
- When an advanced airway is in place (i.e. Endotracheal tube, LMA, King Airway) compressions and ventilations are asynchronous meaning compressions are continuous and the ventilator squeezes the bag very 2-3 seconds for an infant or child.
- It is important to note that the AED should be used as soon as it is available.
- If you are assigning someone other than your partner to call for ALS backup, make sure that person knows you are appointing them for the task. Point if necessary and add descriptive characteristics: "You in the blue shirt, call 911 and tell them that we have an unresponsive adult". This removes confusion that can be caused by the bystander effect, ambiguity, and diffusion of responsibility. Make sure that person stays on the phone, if possible, to update 911 on changes to the patient condition, e.g. CPR has been started.
- When assigning tasks to other rescuers or bystanders, reduce confusion by giving each person a specific goal to work towards. One person can call 911 while another goes to find a defibrillator if one is not available. Giving a bystander multiple tasks increases the chance that one or more of the tasks goes uncompleted.
- If the patient is in a hard to reach or cluttered area, attempt to move the patient to an open space where multiple rescuers and their equipment can easily access and move around. If patient movement would take a long time or is too difficult for you and your partner due to environmental factors or patient weight, either enlist bystanders to assist with movement or treat the patient as best you can.
- While performing compressions, bent elbows can reduce depth and efficacy of compressions and lead to quicker rescuer fatigue. Use bodyweight to compress, not your shoulders/pectorals.
- In the absence of a rescue mask or BVM, The patient can be ventilated via the mouth to mouth technique however this is a judgement call on the rescuer's part as mouth to mouth carries the inherent risk of disease transmission. If you are unwilling or unable to perform mouth to mouth perform hands only CPR (chest compressions only)
- While performing two-person CPR, it may be helpful for the ventilator to count the cycles as the compressor counts compressions out loud. This allows for everyone involved to not only know where you are in the cycle of care but also helps keep track of cycles/shocks so that an accurate count can be given to ALS or the hospital if the patient is transported
Additional Resources[edit | edit source]
- Infant CPR showing mask types
- Infant AED showing pad placement for infant and small child