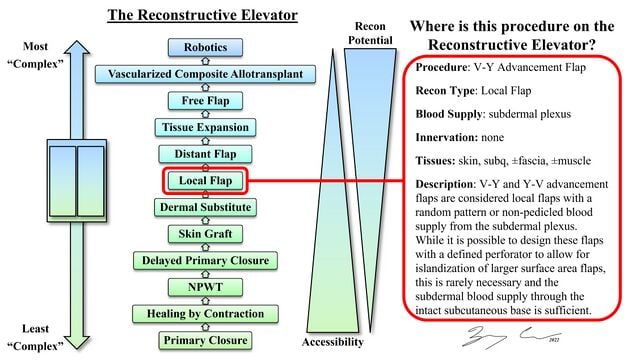
An essential factor to overcoming the global burden of untreated surgical disease is improving access to burn care given the significant impact that burn injuries have on medical and surgical healthcare systems as well as the severe psychosocial and economic ramifications for individuals who receive suboptimal burn care. Women and children from Low-to-Middle SDIs had greater rates of burn incidence, deaths, and DALYs as well as higher mortality ratios with Asia, Sub-Saharan Africa, and the Middle East accounting for most of this morbidity and mortality. V-Y advancement was first described in 1831 by Johann Dieffenbach for the treatment of patients with acquired microstomia. The technique was later modified to its modern islandized conformation by Johannes Esser in 1917. V-Y advancement - and its corollary, Y-V advancement - functions by advancing adjacent tissues to fill small- to medium-cutaneous defects, most often resulting from minor traumas and cutaneous malignancies. V-Y advancement is named for its conversion of a V-shaped incision into a Y-configuration via the advancement of skin and soft tissue in the direction of an adjacent defect. Its corollary - Y-V advancement - represents a modification whereby a Y-shaped incision is converted into a V-configuration via the advancement of skin and soft tissue in the opposite direction. In both cases, healthy skin and soft tissue within the limbs of the flaps are advanced to fill adjacent defects.
Educational Learning Theory
Proposed Learning Theory is a blending of deliberate practice, adaptive flexibility, and Kolb’s Experimental Learning Theory (ELT). Ericsson, Krampe, and Tesch-Römer (1993) established the theoretical framework of deliberate practice. Specifically, the authors (1993) define expert performance as the result of an individuals’ prolonged efforts to improve performance while negotiating motivational and external constraints (p. 363). Moulaert, Verwijnen, Rikers, and Scherpbier, (2004), explain that two distinct motivations are prevalent to mastery skill obtainment motivation and external information. Simply, if a learner is motivated and provided time to utilize outside educational resources (journals, books, videos, etc.) they can achieve proficiency through deliberate practice with the appropriate training materials (2004). Moreover, Ericsson, Prietula, and Cokely, (2007) clearly state the historical evidence that experts are made, not born. Further, their conclusions are based on rigorous research that looked at exceptional performance using scientific methods that are verifiable and most of all reproducible (2007).
Its corollary - Y-V advancement - represents a modification whereby a Y-shaped incision is converted into a V-configuration via the advancement of skin and soft tissue in the opposite direction. In both cases, healthy skin and soft tissue within the limbs of the flaps are advanced to fill adjacent defects.
Prior to proceeding, visit the following pages for foundational content on the general principles of reconstructive surgery:
Flap Design[edit | edit source]
V-Y advancement is named for its conversion of a V-shaped incision into a Y-configuration via the advancement of skin and soft tissue in the direction of an adjacent defect. Its corollary - Y-V advancement - represents a modification whereby a Y-shaped incision is converted into a V-configuration via the advancement of skin and soft tissue in the opposite direction. In both cases, healthy skin and soft tissue within the limbs of the flaps are advanced to fill adjacent defects.
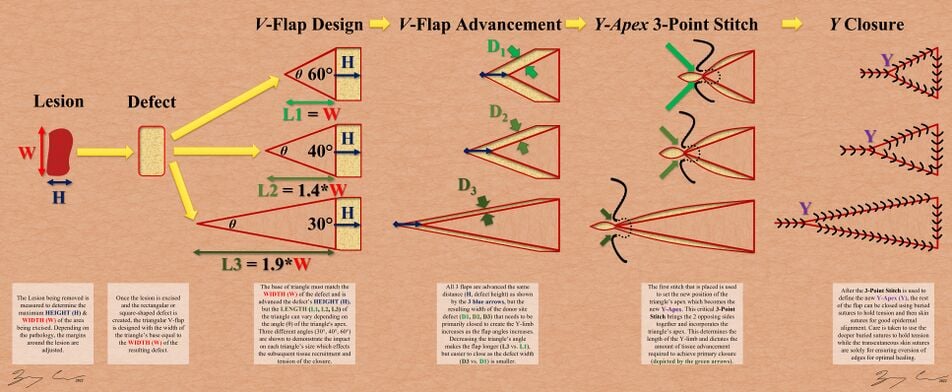
The unilateral V-Y advancement is designed as a triangular flap immediately adjacent to a soft tissue defect. The orientation of the 'V' is designed such that the resulting 'Y' has a central limb that aligns with resting skin tension lines (RSTLs). The angle of the 'V' apex determines the extent of donor site morbidity. That is, a small apex angle results in a long but narrow donor site defect, while a large apex angle results in a short but wide donor site defect. The choice of apex angle is therefore made in consideration of both the available surface area and the laxity of adjacent tissues. If the available surface area is limited by a nearby aesthetic landmark, the apex angle must be made larger so as to minimize flap length. However, tissue laxity must be sufficient to accommodate the wider donor site defect that occurs with a larger apex angle. Alternatively, if tissue laxity is poor, the apex angle can be made smaller so as to minimize donor site width. However, the adjacent surface area must be sufficient to accommodate the longer flap that occurs with a smaller apex angle.
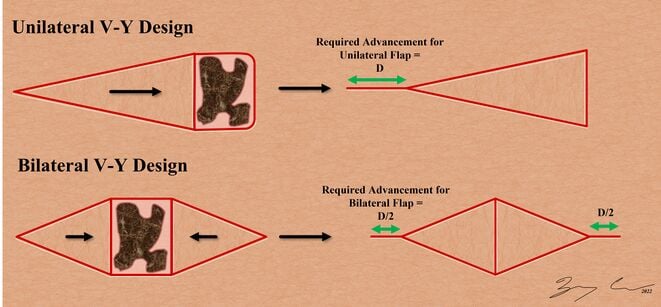
V-Y advancement can also be designed in a bilateral configuration, wherein two separate V-Y advancements are performed on opposite poles of a given defect. Recruitment of healthy tissue into the defect then occurs from either pole. Bilateral V-Y advancement is especially useful for reconstructing wide defects in areas with poor tissue laxity.
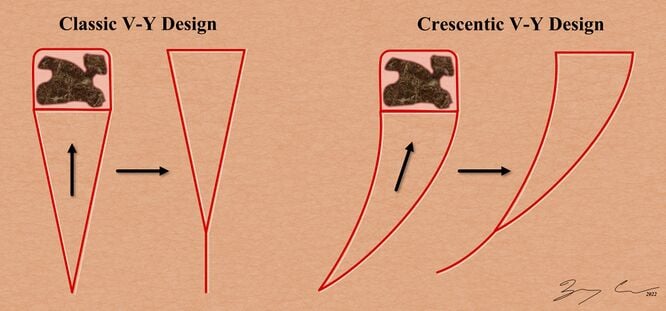
Another common modification of V-Y advancement involves the design of curvilinear V limbs. This allows for the accommodation of nearby aesthetic landmarks and RSTLs.
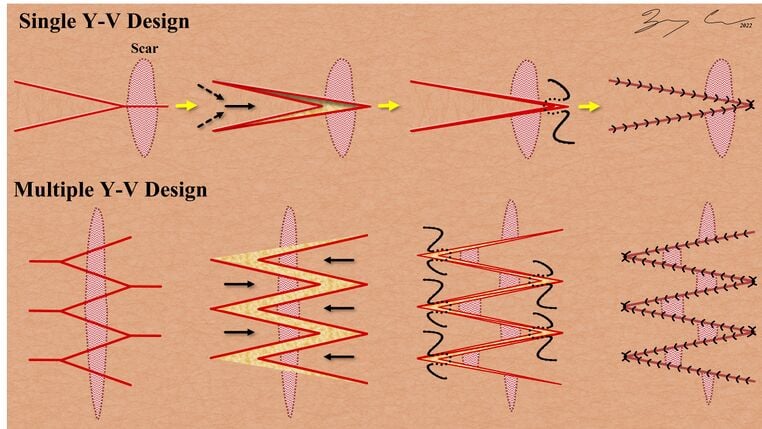
While V-Y advancement is useful for filling adjacent tissue defects, Y-V advancement is useful for dividing adjacent scar contractures. Much like the apex angle in V-Y advancement, the apex angle in Y-V advancement can be altered to modify donor site morbidity. The central limb of the Y-V advancement is designed perpendicular to the scar contracture at hand. The tissue within the Y-shaped incision is then advanced into the divided scar contracture, thereby increasing its length. Multiple Y-V advancements can be designed in parallel to "break up" a scar along its length.
Indications[edit | edit source]
- Close a soft tissue defect originating from burns, trauma, cancer, infections, congenital conditions, or other pathology.
- Release scar contractures (i.e. hypertrophic scars that cross joints, skin tension lines, or cross subunits of the face, breast, and genitalia) and fibrotic cords (i.e. Dupuytren’s Disease).
- Correct webbing, bridle scars, and constriction bands, especially in the neck, popliteal fossa, axilla, extremities, and digits.
- Release of circular contractures around body orifices (e.g. nostril, ear, mouth).
Contraindications[edit | edit source]
- No specific contraindications for this flap.
- If the scar bed is too wide, it will be difficult to achieve closure of the Y-limb and may be best to utilize a different flap that recruits normal tissue from farther away.
Limitations[edit | edit source]
- Requires significant knowledge about skin tension lines and how to assess skin laxity.
- In order to achieve adequate advancement, sufficient skin laxity and adjacent tissue availability is required.
- Dependent upon proper flap design, preservation of subdermal plexus, and thoughtful flap mobilization to avoid ischemia and other wound healing complications.
Instruments[edit | edit source]
- Marking pen
- 15 scalpel
- Toothed adson forceps
- Skin hook
- Needle driver
- Suture
Surgical Technique[edit | edit source]
- Tailor the defect into a rectangular configuration and mark its longest dimension, w
- Draw a line, v, perpendicular to and bisecting w
- Mark the V-apex of the flap along v. Place the V-apex closer to the defect to generate a smaller V-apex angle and accordingly a shorter flap with a wider donor defect. Place the V-apex further from the defect to generate a larger V-apex angle and accordingly a longer flap with narrower donor defect.
- Incise your markings through the epidermis, dermis, and into the subcutaneous tissue
- Elevate the skin adjacent to the flap and the defect so as to facilitate flap inset and donor site closure. Take care NOT to elevate the triangular flap itself so as to preserve its connection with the underlying blood supply.
- Advance the triangular flap into the adjacent defect and secure it in place with two apical simple interrupted sutures
- Place a 3-point buried horizontal mattress suture to approximate the donor site at the V-apex, thereby generating the Y-limb.
- Complete the remainder of the closure using simple interrupted sutures
Complications[edit | edit source]
- Flap necrosis. Flap necrosis most commonly results from the inadvertent undermining of the advancement flap itself. While undermining of adjacent tissues is appropriate to facilitate a tension-free inset, the advancement flap itself must not be divided from its underlying blood supply.
- Dehiscence. Dehiscence most commonly results from improper flap design. If the V-apex angle is made too large, the resulting donor defect will be wide, and its closure will be under undue tension. V-Y advancement dehiscence can also result from poor suture technique or surgical site infection.