This module allows traditional bone setters, pre-hospital providers, clinical officers, nurses, nurse practitioners, and medical officers to become confident and competent in performing point-of-care ultrasound diagnostic imaging to rule out the presence of a pediatric distal forearm fracture and distinguish between buckle (torus) fractures and cortical break fractures to make appropriate referrals as part of the management of closed pediatric (< 16 years of age) distal forearm fractures in regions without access to X-ray imaging and orthopedic specialist coverage.[1][2][3][4][5][6][7][8][9]
Learning Objectives[edit | edit source]
- Identify the primary sonographic features of no fracture, a buckle (torus) fractures and a cortical break fracture of the pediatric distal forearm
- Describe the secondary sonographic features of a cortical break fracture of the pediatric distal forearm
- Perform the 6 view method for ultrasonographic diagnosis of pediatric distal forearm fractures
- Practise conducting a bilateral ultrasound scan to diagnose a pronator quadratus hematoma
Sonographic Features of Pediatric Distal Forearm Fractures[edit | edit source]
| Sonographic Features of Pediatric Distal Forearm Bones | # | Fracture Subtype | Fracture Description | Sonographic Signs | Ultrasound Image |
|---|---|---|---|---|---|
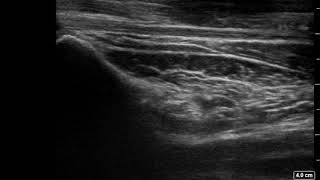
| 1 | No Fracture | "Unbroken" |
|
 | |
| 2 | Buckle (Torus) Fracture | "Bent" | 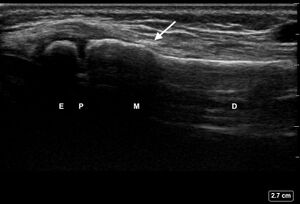 | ||
| 3 | Cortical Break Fracture | "Broken" | Break, step or gap in bone cortex which appears as a black zone in the bright, sharp white line[10][11][14][15][16] | 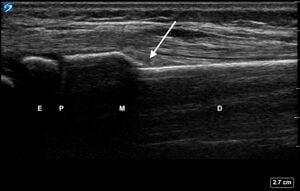 |
Secondary Signs of Pediatric Distal Forearm Cortical Break Fractures[edit | edit source]
Any of these secondary signs should prompt a closer look for a cortical break fracture on all views and potential referral for X-ray imaging.
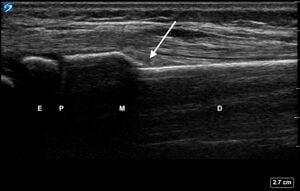
| Secondary Signs of Pediatric Distal Forearm Cortical Break Fractures | # | Sonographic Signs | Ultrasound Image |
|---|---|---|---|
| 1 | Angulation of the distal bone segment[14] | 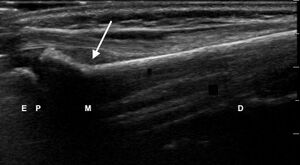 | |
| 2 | Fracture < 1 cm from physis |  | |
| 3 | Periosteal hematoma[14][15] |  | |
| 4 | Pronator quadratus hematoma[17][14][18] |  |
Ultrasound Basic Skills[edit | edit source]
- Fanning the iQ
- Sliding the iQ
- Rotating the iQ
- Proper Hand Positioning
- Choosing the Right Preset
- Adjusting the Overall Gain
6 View Technique for Ultrasound Scanning of Pediatric Distal Forearm Fractures[edit | edit source]
| 6 View Technique for Ultrasound Scanning of Pediatric Distal Forearm Fractures | # | Procedure Step | Reference Multimedia |
|---|---|---|---|
| 1 |
|
||
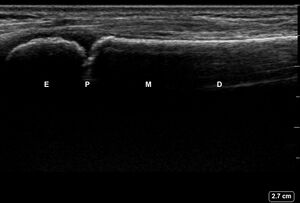
| 2 | Obtain, label, and save an image of the epiphysis (E), physis (P), metaphysis (M), and diaphysis (D). |  | |
| 3 | Obtain, label, and save an image of any primary or secondary sonographic signs of a buckle or cortical break fracture; including:
|
 | |
| 4 | Repeat steps 1-3 for the dorsal aspect of the ulna. | 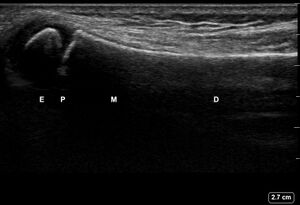 | |
| 5 | Repeat steps 1-3 for the lateral aspect of the ulna. | 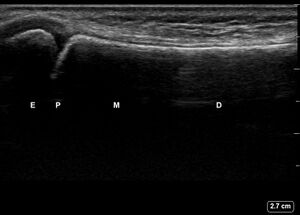 | |
| 6 | Repeat steps 1-3 for the lateral aspect of the radius. |  | |
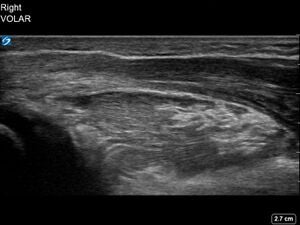
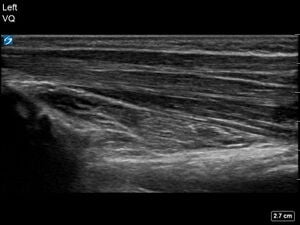
| 7 | Allow the patient to gently supinate their forearm to at least 90 degrees to access the volar (palmar) aspect of the distal forearm. |  | |
| 8 | Repeat steps 1-3 for the volar (palmar) aspect of the radius. |  | |
| 9 | Repeat steps 1-3 for the volar (palmar) aspect of the ulna. |  |
Ultrasound Scanning for Pronator Quadratus Hematoma Sign[edit | edit source]
Record a 4 second video while slowly sweeping across the volar (palmar) aspect of the distal forearm until the metaphysis of the distal ulna is in the field of view.
Acknowledgements[edit | edit source]
This work is funded by a grant from the Intuitive Foundation. Any research, findings, conclusions, or recommendations expressed in this work are those of the author(s), and not of the Intuitive Foundation.
References[edit | edit source]
- ↑ Onyemaechi NO, Itanyi IU, Ossai PO, Ezeanolue EE. Can traditional bonesetters become trained technicians? Feasibility study among a cohort of Nigerian traditional bonesetters. Hum Resour Health. 2020 Mar 20;18(1):24. doi: 10.1186/s12960-020-00468-w. PMID: 32197617; PMCID: PMC7085192.
- ↑ Heiner JD, McArthur TJ. The ultrasound identification of simulated long bone fractures by prehospital providers. Wilderness Environ Med. 2010 Jun;21(2):137-40. doi: 10.1016/j.wem.2009.12.028. Epub 2009 Dec 22. PMID: 20591377.
- ↑ Heiner JD, Baker BL, McArthur TJ. The ultrasound detection of simulated long bone fractures by U.S. Army Special Forces Medics. J Spec Oper Med. 2010 Spring;10(2):7-10. PMID: 20936597.
- ↑ Heiner JD, Proffitt AM, McArthur TJ. The ability of emergency nurses to detect simulated long bone fractures with portable ultrasound. Int Emerg Nurs. 2011 Jul;19(3):120-4. doi: 10.1016/j.ienj.2010.08.004. Epub 2010 Sep 25. PMID: 21665155.
- ↑ Snelling PJ, Jones P, Keijzers G, Bade D, Herd DW, Ware RS. Nurse practitioner administered point-of-care ultrasound compared with X-ray for children with clinically non-angulated distal forearm fractures in the ED: a diagnostic study. Emerg Med J. 2021 Feb;38(2):139-145. doi: 10.1136/emermed-2020-209689. Epub 2020 Sep 8. PMID: 32900856.
- ↑ Snelling PJ, Jones P, Moore M, Gimpel P, Rogers R, Liew K, Ware RS, Keijzers G. Describing the learning curve of novices for the diagnosis of paediatric distal forearm fractures using point-of-care ultrasound. Australas J Ultrasound Med. 2022 Mar 7;25(2):66-73. doi: 10.1002/ajum.12291. PMID: 35722050; PMCID: PMC9201201.
- ↑ Heiner JD, McArthur TJ. A simulation model for the ultrasound diagnosis of long-bone fractures. Simul Healthc. 2009 Winter;4(4):228-31. doi: 10.1097/SIH.0b013e3181b1a8d0. PMID: 19915442.
- ↑ Snelling PJ, Keijzers G, Byrnes J, Bade D, George S, Moore M, Jones P, Davison M, Roan R, Ware RS. Bedside Ultrasound Conducted in Kids with distal upper Limb fractures in the Emergency Department (BUCKLED): a protocol for an open-label non-inferiority diagnostic randomised controlled trial. Trials. 2021 Apr 14;22(1):282. doi: 10.1186/s13063-021-05239-z. PMID: 33853650; PMCID: PMC8048294.
- ↑ Snelling PJ. A low-cost ultrasound model for simulation of paediatric distal forearm fractures. Australas J Ultrasound Med. 2018 Feb 25;21(2):70-74. doi: 10.1002/ajum.12083. PMID: 34760505; PMCID: PMC8409885.
- ↑ 10.0 10.1 10.2 10.3 Saul T, Ng L, Lewiss RE. Point‐of‐care ultrasound in the diagnosis of upper extremity fracture‐dislocation. A pictorial essay. Med Ultrason 2013; 15(3): 230–6.
- ↑ 11.0 11.1 11.2 Snelling PJ. A low-cost ultrasound model for simulation of paediatric distal forearm fractures. Australas J Ultrasound Med. 2018 Feb 25;21(2):70-74. doi: 10.1002/ajum.12083. PMID: 34760505; PMCID: PMC8409885.
- ↑ [Peer-Reviewed, Web Publication] Chodakowski J, Weygandt L. (2019, April 28). Ultrasound in pediatric distal forearm fractures. [NUEM Blog. Expert Commentary by Haney R]. Retrieved from http://www.nuemblog.com/blog/us-for-fracture
- ↑ Saul T, Ng L, Lewiss RE. Point-of-care ultrasound in the diagnosis of upper extremity fracture-dislocation. A pictorial essay. Med Ultrason. 2013 Sep;15(3):230-6. doi: 10.11152/mu.2013.2066.153.ts1ln2. PMID: 23979619.
- ↑ 14.0 14.1 14.2 14.3 14.4 Snelling PJ, Keijzers G, Byrnes J, Bade D, George S, Moore M, Jones P, Davison M, Roan R, Ware RS. Bedside Ultrasound Conducted in Kids with distal upper Limb fractures in the Emergency Department (BUCKLED): a protocol for an open-label non-inferiority diagnostic randomised controlled trial. Trials. 2021 Apr 14;22(1):282. doi: 10.1186/s13063-021-05239-z. PMID: 33853650; PMCID: PMC8048294.
- ↑ 15.0 15.1 15.2 Herren C, Sobottke R, Ringe MJ, et al. Ultrasound-guided diagnosis of fractures of the distal forearm in children. Orthop Traumatol Surg Res 2015; 101:501.
- ↑ 16.0 16.1 Pountos I, Clegg J, Siddiqui A. Diagnosis and treatment of greenstick and torus fractures of the distal radius in children: a prospective randomised single blind study. J Child Orthop 2010; 4: 321–6.
- ↑ Snelling PJ, Keijzers G, Ware RS. Point-of-care ultrasound pronator quadratus hematoma sign for detection of clinically non-angulated pediatric distal forearm fractures: a prospective cohort study. J Ultrasound Med 2022; 41(1): 193–205.
- ↑ Snelling PJ, Keijzers G, Ware RS. Point-of-Care Ultrasound Pronator Quadratus Hematoma Sign for Detection of Clinically Non-Angulated Pediatric Distal Forearm Fractures: A Prospective Cohort Study. J Ultrasound Med. 2022 Jan;41(1):193-205. doi: 10.1002/jum.15695. Epub 2021 Mar 10. PMID: 33749859.