This module allows traditional bone setters, pre-hospital providers, clinical officers, nurses, nurse practitioners, and medical officers to become confident and competent in performing point-of-care ultrasound diagnostic imaging to rule out the presence of a pediatric distal forearm fracture and distinguish between buckle (torus) fractures and cortical break fractures to make appropriate referrals as part of the management of closed pediatric (< 16 years of age) distal forearm fractures in regions without access to X-ray imaging and orthopedic specialist coverage.[1][2][3][4][5][6][7][8][9] These 3D printed bone models feature a semi-engraved model number, gender symbol, and two mould insertion direction arrows on the base of each model to assist with model identification and proper orientation of each bone model in the mould.
3D Printed Pediatric Female Forearm Simulator Mould[edit | edit source]
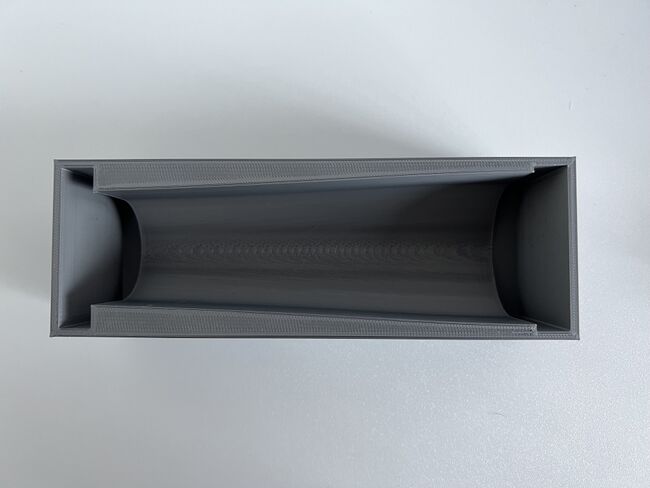
The 3D Printed Pediatric Female Forearm Simulator Mould is designed as a reusable, open-face, negative mould so the assembled bone model can be inserted into the rectangular mould and a bisected funnel-shaped gelatin shell can be created around the bone model. The interior of the mould is lined with clear cellophane wrap before a gelatine solution is poured into the mould.
3D Printing Software, Hardware, and Filament Specifications[edit | edit source]
All 4 requirements below must be met in order to digitally manufacture the 3D Printed Pediatric Female Forearm Simulator Mould.
- 3D Printer Type: Fused Filament Fabrication
- Minimum Build Plate Dimensions: 230 mm wide
- Printer Enclosure: to prevent filament warping
- Filament: PLA (any colour)
Download Ready-To-Print GCODE Files[edit | edit source]
If you have a Prusa i3MK3S 3D printer, please download the ready-to-print g-code file below.
Prusa i3MK3S 3D Printer[edit | edit source]
Table 1. Pediatric Female Distal Forearm Simulator Mould GCODE Files for Prusa i3MK3S 3D Printer
| Model Number | Print Time | PLA Filament Weight | Download G-CODE File | Revision Date |
|---|---|---|---|---|
| 1 | 14 hours, 39 minutes | 244 grams | Click here to download g-code or right-click this link and select "Save link as:" File name: Mould - Female - Prusa i3MK3S - 6-Nov-2022 version and Save as type: .GCODE File | November 6 2022 |
Download 3D Model File For Slicing[edit | edit source]
Download the 3D file (.STL) in the table below to input the required print settings to create the print file (.GCODE) for other 3D printers.
Table 2. 3D Printed Pediatric Forearm Simulator Mould 3D File
| Download STL File | Revision Date |
|---|---|
| Click on this link and click on "Mould_-_Female_-6-Nov-2022_version.stl" to download the file | November 6, 2022 |
Input Required Print Settings[edit | edit source]

Please pay attention to and input all the required settings below to ensure the mould prints properly.
- Filament Material: PLA at default settings
- Support: None
- Layer Height: 0.2 mm or less
- Bed Temperature: Minimum 55 degrees Celsius
- Model Orientation: Rectanglar base of mould lays flat on build plate
Inspect Mould Before Use or Delivery[edit | edit source]
- Ensure the mould interior is smooth and free of any sharp edges that could puncture the cellophane lining and lead to gelatine leakage during use.
- Inspect the mould exterior to identify any potential leakage sites. If any potential leakage sites are present, do not pour gelatine into the mould.
Acknowledgements[edit | edit source]
This work is funded by a grant from the Intuitive Foundation. Any research, findings, conclusions, or recommendations expressed in this work are those of the author(s), and not of the Intuitive Foundation.
References[edit | edit source]
- ↑ Onyemaechi NO, Itanyi IU, Ossai PO, Ezeanolue EE. Can traditional bonesetters become trained technicians? Feasibility study among a cohort of Nigerian traditional bonesetters. Hum Resour Health. 2020 Mar 20;18(1):24. doi: 10.1186/s12960-020-00468-w. PMID: 32197617; PMCID: PMC7085192.
- ↑ Heiner JD, McArthur TJ. The ultrasound identification of simulated long bone fractures by prehospital providers. Wilderness Environ Med. 2010 Jun;21(2):137-40. doi: 10.1016/j.wem.2009.12.028. Epub 2009 Dec 22. PMID: 20591377.
- ↑ Heiner JD, Baker BL, McArthur TJ. The ultrasound detection of simulated long bone fractures by U.S. Army Special Forces Medics. J Spec Oper Med. 2010 Spring;10(2):7-10. PMID: 20936597.
- ↑ Heiner JD, Proffitt AM, McArthur TJ. The ability of emergency nurses to detect simulated long bone fractures with portable ultrasound. Int Emerg Nurs. 2011 Jul;19(3):120-4. doi: 10.1016/j.ienj.2010.08.004. Epub 2010 Sep 25. PMID: 21665155.
- ↑ Snelling PJ, Jones P, Keijzers G, Bade D, Herd DW, Ware RS. Nurse practitioner administered point-of-care ultrasound compared with X-ray for children with clinically non-angulated distal forearm fractures in the ED: a diagnostic study. Emerg Med J. 2021 Feb;38(2):139-145. doi: 10.1136/emermed-2020-209689. Epub 2020 Sep 8. PMID: 32900856.
- ↑ Snelling PJ, Jones P, Moore M, Gimpel P, Rogers R, Liew K, Ware RS, Keijzers G. Describing the learning curve of novices for the diagnosis of paediatric distal forearm fractures using point-of-care ultrasound. Australas J Ultrasound Med. 2022 Mar 7;25(2):66-73. doi: 10.1002/ajum.12291. PMID: 35722050; PMCID: PMC9201201.
- ↑ Heiner JD, McArthur TJ. A simulation model for the ultrasound diagnosis of long-bone fractures. Simul Healthc. 2009 Winter;4(4):228-31. doi: 10.1097/SIH.0b013e3181b1a8d0. PMID: 19915442.
- ↑ Snelling PJ, Keijzers G, Byrnes J, Bade D, George S, Moore M, Jones P, Davison M, Roan R, Ware RS. Bedside Ultrasound Conducted in Kids with distal upper Limb fractures in the Emergency Department (BUCKLED): a protocol for an open-label non-inferiority diagnostic randomised controlled trial. Trials. 2021 Apr 14;22(1):282. doi: 10.1186/s13063-021-05239-z. PMID: 33853650; PMCID: PMC8048294.
- ↑ Snelling PJ. A low-cost ultrasound model for simulation of paediatric distal forearm fractures. Australas J Ultrasound Med. 2018 Feb 25;21(2):70-74. doi: 10.1002/ajum.12083. PMID: 34760505; PMCID: PMC8409885.